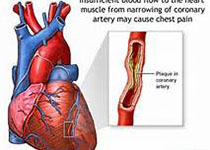
JACC:脂蛋白水平能否预测女性心血管疾病发生风险?
2018-07-14 MedSci MedSci原创
脂蛋白(a)[Lp(a)]虽然已证实与心血管疾病(CVD)的发生相关,但其对CVD的预测价值尚存在争议。本研究的目的旨在评估Lp(a)在女性CVD发生中的临床预测价值。本研究纳入了来自WHS临床研究中的24558名女性、WHI临床研究中的1815名女性、JUPITER临床研究中的2569名女性和5161名男性,通过浊度测定法对其进行了Lp(a)含量测定。分析结果显示,在WHS临床研究中,Lp(a)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#JACC#
34
学习了,,,
73
学习了谢谢分享
63
学习学习.谢谢分享!
71
#ACC#
34
#脂蛋白#
25
#血管疾病#
21
学习了.谢谢分享
89
好
56