Nat Commun:新型候选药物或能利用新型吸收策略来靶向作用小鼠机体中的癌细胞
2022-08-24 生物谷 生物谷
这篇研究报告中,研究人员报道了一种新型激酶抑制剂,其或能明显减少疾病、限制毒性作用并延长骨髓纤维化小鼠的生存期,骨髓纤维化是急性白血病的前期形式。
激活癌症中的补偿信号节点通常需要联合疗法,且联合治疗通常受到了剂量限制毒性副作用的困扰。近日,一篇发表在国际杂志Nature Communications上题为“A lymphatic-absorbed multi-targeted kinase inhibitor for myelofibrosis therapy”的研究报告中,来自密歇根大学等机构的科学家们通过研究开发出了一种新型的抗癌药物,其或能通过肠道的淋巴系统而并非是血管来吸收的,这或许能超越导致药物耐受性的分子信号通路,同时还会增加机体的抗癌能力并降低药物所产生的副作用。
这篇研究报告中,研究人员报道了一种新型激酶抑制剂,其或能明显减少疾病、限制毒性作用并延长骨髓纤维化小鼠的生存期,骨髓纤维化是急性白血病的前期形式。文章中,研究人员设计了一种名为LP-182的口服药物,其或能同时靶向作用名为PI3K的磷酸肌肽3-激酶以及有丝分裂激活的蛋白激酶MAPK,后者是一种能驱动较高比例癌症的特殊分子信号通路。
癌症疗法通常会涉及组合性疗法来靶向作用不同癌细胞的易感性,但由于这些药物会在体内循环并以不同的速度被吸收和清除,因此在限制药物毒性作用和其副作用的同时,以一种有效的必要浓度来维持每种药物的正确治疗平衡就显得急剧挑战性了。如果无法取得这种平衡,或许就会降低药物组合抵御癌症的有效性,并导致药物耐受性的发生,比如PI3K和MAPK之间的串扰或许就会激活下游通路对疗法的抵抗,即使一种药物阻断了其中一种途径,另一种途径也能提供一种逃逸的生存途径来补偿并继续生长。
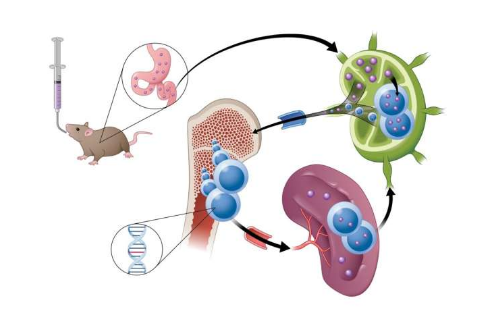
新型候选药物或能利用新型吸收策略来靶向作用小鼠机体中的癌细胞。
图片来源:Danielle Dobbs/Michigan Medicine
与传统口服药物(其通常被设计能快速吸收到血液中)不同,研究人员在治疗患有骨髓纤维化的小鼠时发现,LP-182能首先被肠道中的淋巴系统吸收,这种淋巴系统能充当一种储存库的角色,将药物与机体其它部位分开,并随着时间推移不断将疗法释放到机体一般的循环中,同时保持药物浓度在最佳的治疗性水平下。研究者Ross说道,在治疗窗口期内,我们就能保持对两种能相互对话的不同通路的靶向抑制作用,这或许就证明了将抗癌药物制剂直接运输到淋巴系统内的可行性,从而就能提供新的机会来改善癌症疗法的治疗效果并降低药物本身所带来的副作用。在骨髓纤维化中,过多的疤痕组织会在骨髓中形成,从而破坏正常的血细胞产生,过度活跃的分子信号会导致恶性干细胞的增殖以及广泛的纤维化、脾脏肿大以及进行性的骨髓衰竭。
这种疾病会通过淋巴组织来扩散,同时其也是癌症发生转移的一个常见途径,因此研究人员的最新研究或许就为预防癌症扩散提供了新的策略,此外,由于肠道淋巴系统中拥有近乎一半机体的免疫细胞,本文研究结果或能为开发治疗自身免疫性疾病和其它疾病的新型疗法提供新的策略。
后期研究者Ross及其同事还将继续深入研究来扩大对LP-182的临床研究,旨在对骨髓纤维化人类患者开展I期临床试验,目前研究人员还正在开发更多的淋巴靶向性激酶抑制剂从而治疗更多实体瘤,比如乳腺癌、脑癌、胃肠道和胰腺癌等,以及诸如狼疮和多发性硬化症等自身免疫性疾病。
原始出处:
Ross, B.D., Jang, Y., Welton, A. et al. A lymphatic-absorbed multi-targeted kinase inhibitor for myelofibrosis therapy. Nat Commun 13, 4730 (2022). doi:10.1038/s41467-022-32486-8
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#靶向作用#
45
#COMMUN#
52
#Nat#
41
#候选药物#
49
#癌细胞#
60