肺动脉高压引起右心衰竭的病理生理学
2021-12-03 刘少飞 MedSci原创
当心脏的 RV 无法将血液泵送到肺部以满足需求时,这种情况称为 RVF。由于解剖学和生理学上的差异,两个心室对压力的反应相反。迄今为止,可用于 RVF 的传统疗法无法提供任何令人信服的结果。
右心室衰竭 (RVF) 的特征是心脏的右心室 (RV) 受损,无法有效地将血液泵送到肺部,而肺部又会积聚在静脉中。多表现:液体积聚进展为外周水肿、全身水肿、腹水;室性和房性心律失常;由于心输出量减少,运动耐量和疲劳度下降。近二十年来,越来越多的研究强调了RV的重塑及其在广泛的心血管疾病中的应用。然而,它是一个相对年轻的领域。在表现出传统HF症状的患者的治疗管理和诊断评估方面,RVF知之甚少。随着时间的推移,辅助性RV功能障碍所起的突出作用已得到承认。这在患有RVF的患者中可能很明显,尽管通过LV辅助装置 (LVAD) 对LV进行了血流动力学监测,但已经注意到死亡率和发病率显着增加。然而,除了肺血管阻力和RV后负荷升高导致RV扩张和功能障碍的肺动脉高压除外,研究RV在有症状的HF患者中的作用的兴趣稍低。
尽管努力有所改善,但RVF仍然是一个主要的公共卫生问题。在危重患者中,RV功能障碍主要是呼吸衰竭或肺动脉高压 (PH) 的结果。通常肺动脉高压会导致RVF。通常称为肺心病,它是由肺部疾病特别是肺栓塞引起的 RVF 发病率,这是一种常见的疾病,导致大约 5-10% 的危重患者死亡。RVF是心脏移植后和其他心胸手术初始阶段死亡率的主要因素。有大量数据提供了关于左心室 (LV) 肥厚进展为 LV 衰竭的潜在机制的令人信服的看法。相比之下,由于容量或压力过载导致的右心室 (RV) 反馈的可用数据很少。先进的成像技术有助于研究 RV 的生理学、解剖学和患病状态。然而,右心室衰竭 (RVF) 的治疗方案需要更多关注。它是类癌综合征、肺动脉高压、房间隔缺损和其他几种伴随疾病患者的关键临床风险。尽管舒张末期压力增加时两个心室的重构反应基本相同,受压的 RV 变得更容易发生氧化应激,从而激活血管生成减少的凋亡机制。与 LV 相比,这促使 RV 向失败发展。经验性心力衰竭 (HF) 疗法在改善患者的死亡率和心功能方面无效,这促使 RVF 和 LV 衰竭的潜在病理生理学之间存在差异。应设计治疗策略,同时考虑 RV 的解剖学和生理学特征。
RVF的病理生理学
心脏的RV是一个独特的腔室,具有独特的解剖学和生理学。它与肺循环和体静脉回流有关。它的主要作用是将血液泵入肺循环。RV功能与心脏收缩力、后负荷、前负荷、心律和LV功能相关。右心房压和全身充盈压是决定静脉回流的两个参数。然而,在肺循环中,与体循环相比,所需的压力要小得多;由于移动相同量的血液,与LV相比,大约四分之一的每搏功是由RV产生的。因此,与 LV 的壁厚相比,RV 的壁厚要小得多。考虑到同一阶段 LV 的近似厚度为 8-11 毫米,通常它在舒张末期不超过 2-3 毫米。由于静脉回流的波动,RV 更具延展性(约 10-15%),允许它根据不同的静脉回流量进行调整,而舒张末压没有任何变化。
RV 的一个重要特征是它对后负荷的微小变化的显着反应。后负荷的突然增加会导致 RV 扩张以维持每搏输出量。已经进行了一项实验研究,该研究指出左侧和 RV 对后负荷变化的反应存在差异。虽然前者表现出每搏量的轻微下降,但后者表现出每搏量的显着下降。另一个主要现象是心室相互依存,表现为 RV 容量超负荷时 LV 的容量压缩和 D 形(图下)。心包膜进一步增强了这一点。因此,LV 每搏输出量的间接减少是明显的。
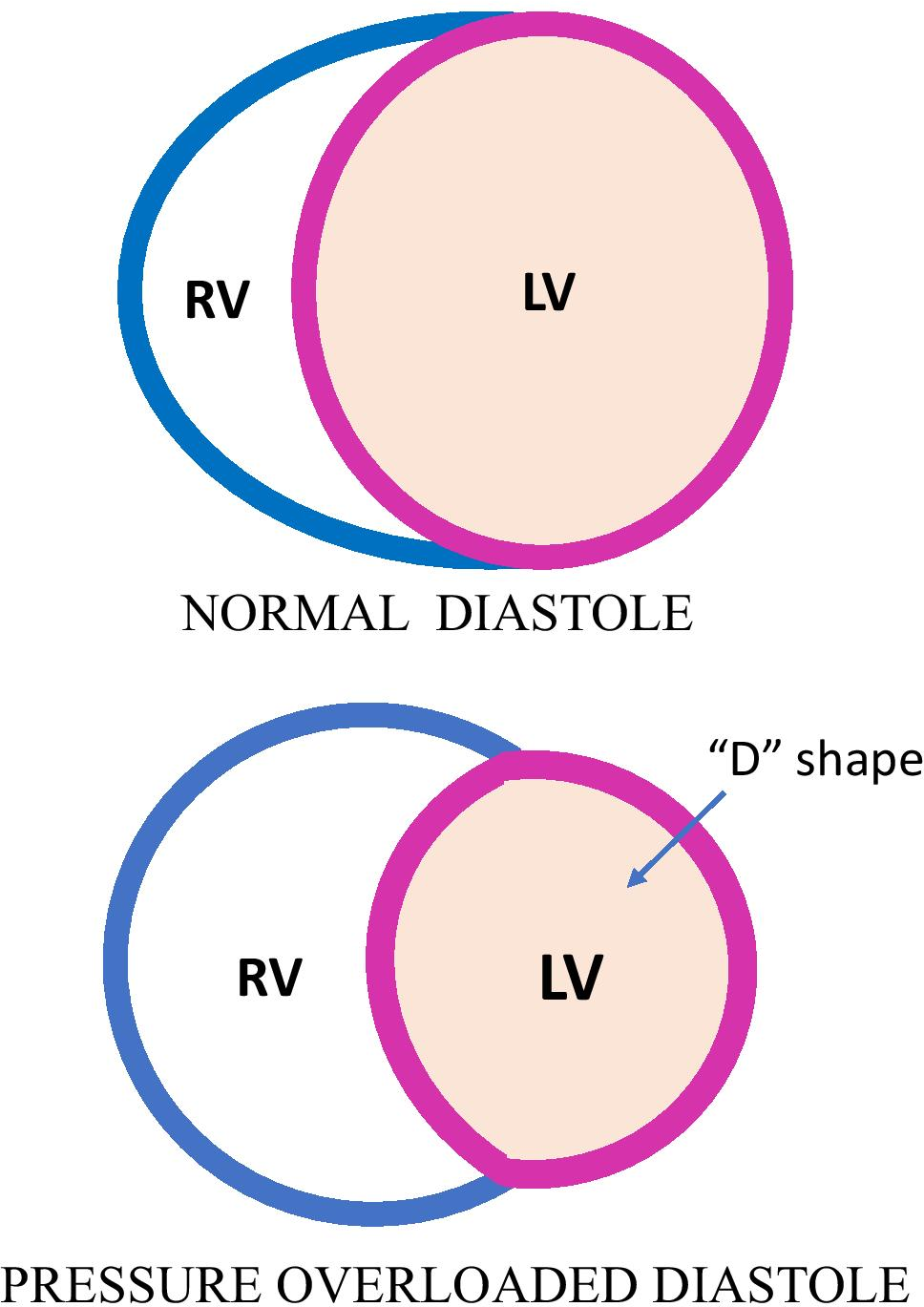
正常和患病状态下的心室解剖。由于心室相互依存,RV 压力超负荷导致 LV 容积压缩和 D 形。
除了心室相互依赖之外,正常 RV 功能的主要决定因素主要是前负荷和后负荷、收缩力和心律。在这些因素中发现的差异表明新的或预先存在的肺部或心脏疾病,或两者的组合,最终导致 RVF。
有多种因素会导致 RV 承受压力,如容量或压力超负荷、MI 或心包疾病。它最初会对 RV 造成轻微伤害或对心肌造成压力,随着时间的推移逐渐加重。慢性 LV 功能障碍是 RVF 背后的主要因素。此外,PH 在引起 RVF 方面也具有重要意义。RV 功能障碍也是先天性心脏病的结果,如法洛四联症、艾森曼格综合征和埃布斯坦异常。
增加压力对 RV 的影响
在收缩末期压力升高时,随着 LV 和 RV 射血分数的降低,会注意到收缩末期容积的增加。在这种环境下,随着射血分数的降低,心输出量显着减少,同时每搏输出量减少。为了对抗这种情况以维持心输出量,RV 表现出收缩状态的增加。这种由于需求增加而导致的收缩性快速激增被称为 Anrep 效应或自律自动调节,它主要由钙动力学介导,而肾上腺素能状态没有任何改变。随着后负荷的进一步升高,RV 腔会扩张,并且在某个时间点之后,RV 收缩力会突然、剧烈、不可逆转地下降。这是 RV 无法代偿的点,可以看到心输出量和全身压力显着降低 。RV 缺血加剧了这种塌陷。然而,由于压力过载,它并不是 RV 收缩功能发生改变的唯一原因。事实上,它在大多数肺心病患者中甚至可能并不显着. 在人类和动物研究中,压力超负荷状态下不透明的心肌结缔组织会导致明显的组织学变化。在急性 RV 压力超负荷状态后,在 RV 游离壁中会出现明显的超微结构变化,如局灶性肌细胞坏死。这可能是由于肌原纤维的机械破坏或肾上腺素能系统的过度刺激。通常蛋白酶如钙蛋白酶在 RV 功能障碍中起作用,这在骨骼肌中很明显。相比之下,RV 可以很好地耐受两种慢性压力超负荷状态,包括先天性肺动脉狭窄和艾森曼格综合征。
简而言之,需要更多地了解 RV 功能障碍背后的潜在机制。更好的诊断介质、血液动力学监测和非侵入性成像技术是最佳治疗的必要条件。考虑到 RVF 在临界条件下的随机发生,该领域需要更多的研究和调查。
参考文献”
Das P, Thandavarayan RA, Watanabe K, Velayutham R, Arumugam S. Right ventricular failure: a comorbidity or a clinical emergency? Heart Fail Rev. 2021 Nov 26. doi: 10.1007/s10741-021-10192-9. Epub ahead of print. PMID: 34826024.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#病理生理#
55
#生理学#
39
#动脉高压#
47
#心衰竭#
48
#右心衰竭#
44
#病理生理学#
34
#右心衰#
40