Nat Commun:科学家发现乳腺癌扩散的罪魁祸首“高胆固醇”,确定新的药物靶点
2017-10-13 佚名 medicalxpress
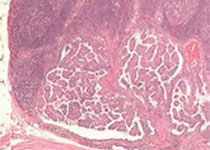
高胆固醇水平与乳腺癌扩散到身体其他部位有关,但医生和研究人员并不知道这一联系的原因。伊利诺伊大学(UniversityofIllinois)的一项新的研究发现,罪魁祸首是胆固醇代谢的副产品,它作用于特定的免疫细胞,从而促进癌细胞的扩散,而不是阻止癌细胞扩散。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Nat#
21
#科学家发现#
20
#COMMUN#
18
#药物靶点#
41
henhao
67