JACC:传统外科生物瓣膜置换术 vs 快速瓣膜释放术
2018-03-28 MedSci MedSci原创
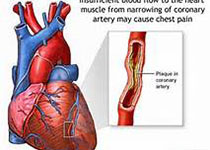
目前,对于主动脉瓣疾病的患者,外科的传统生物瓣膜置换(CBVs)手术是治疗的标准,但是近期也出现了新式的快速释放瓣膜(RDVs)手术。本研究的目的旨在评估和比较RDVs和CBVs在治疗主动脉瓣狭窄患者中的疗效。本研究纳入了数据库中2011年至2015年接受外科主动脉瓣置换术(RDVs或者CBVs)的22062名患者,并通过1:1的倾向评分匹配比较了RDVs和CBVs患者的各类参数。最终共有2093
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#置换#
28
#生物瓣#
32
#JACC#
34
学习了.谢谢作者分享!
66
#瓣膜置换术#
46
#ACC#
30
#生物瓣膜#
31
#置换术#
28
#瓣膜#
30
不错耶.学习了
50