JACC:梗阻性肥厚型心肌病患者的心肌组织病理与临床特征的相关性
2021-05-04 Nebula MedSci原创
对于梗阻性肥厚型心肌病患者,组织病理学结果与临床表现有关,包括发病年龄和心律失常
肥厚型心肌病(HCM)是一种遗传性心肌病,以心肌细胞肥大、心肌细胞紊乱、间质纤维化等多种病理特征为特点。
本研究尝试将梗阻性肥厚性心肌病患者的临床特征和室间隔心肌切除术后的预后与心肌组织病理学联系起来。
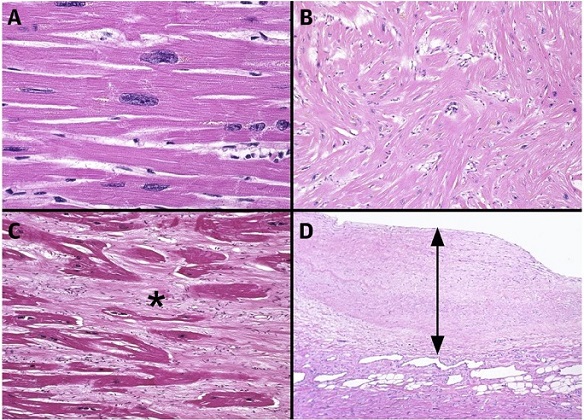
研究人员回顾了2000-2016年间接受室间隔心肌切除术的1836例梗阻性肥厚型心肌梗死患者术后的心肌病理结果。对心肌细胞肥大、心肌细胞紊乱、间质纤维化和心内膜增厚进行分级和分析。
HCM患者的心脏病理:A 心肌细胞肥大,B 心肌细胞紊乱,C 间质纤维化,D 心内膜增厚
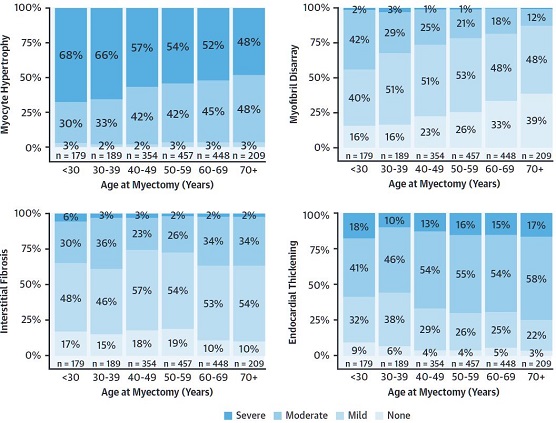
纳入分析的患者的中位年龄为54.2岁(43.5~64.3岁),1067例男性(58.1%)。心肌细胞紊乱与手术时的年龄之间存在微弱的负相关(ρ=-0.22, p<0.001)。心肌细胞肥大(p<0.001)、心肌细胞紊乱(p<0.001)和间质纤维化(p<0.001)都与植入型心律转复除颤器植入率呈正相关。间质纤维化(p<0.001)和心内膜增厚(p<0.001)均与术前心房颤动相关。
不同年龄组的心肌组织病理特征
在COX生存模型中,年龄较大(p<0.001)、心肌细胞肥大程度较低(重度 vs 轻度,危险比:0.41;95%CI 0.19~0.86;p=0.040)和较低程度心内膜增厚(中度 vs 轻度,危险比:0.75;95%CI 0.58~0.97;p=0.019)均与室间隔心肌切除术后较差的生存独立相关。
在进行基因型分析的256例患者中,具有致病或可能致病变异的患者(n=62)的心肌细胞紊乱程度更严重(42% vs 15% vs 20%;p=0.022)。值得注意的是,13例具有致病或可能致病基因变异的HCM患者没有心肌细胞紊乱。
总之,对于梗阻性肥厚型心肌病患者,组织病理学结果与临床表现有关,包括发病年龄和心律失常。心肌细胞肥大和心内膜增厚与室间隔心肌切除术后的死亡率呈负相关。
原始出处:
Cui Hao,Schaff Hartzell V,Lentz Carvalho Juliano et al. Myocardial Histopathology in Patients With Obstructive Hypertrophic Cardiomyopathy. J Am Coll Cardiol, 2021, 77: 2159-2170.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#JACC#
28
#梗阻性肥厚型心肌病#
38
#临床特征#
38
#相关性#
27
学习了
52
#ACC#
23
#肌病#
25
非常值得学习的知识,学习使人进步
59