Cell Repo:FoxM1与乳腺癌发生的关系
2012-06-18 mili 生物谷
FoxM1(Forkhead box protein M1)是一个癌蛋白,在乳腺癌中,FoxM1高表达总是与较差的愈后和细胞分化不完全有关。但FoxM1是如何调节乳腺细胞分化的目前尚不清楚。 本文的研究者发现,FoxM1以转录抑制因子的身份,来调节管腔上皮祖细胞分化的。在乳腺再生的过程中高表达FoxM1会导致管腔上皮祖细胞数量增多和乳腺导管形态紊乱。与之相反,敲减FoxM1则会导致乳腺细胞的过度
FoxM1(Forkhead box protein M1)是一个癌蛋白,在乳腺癌中,FoxM1高表达总是与较差的愈后和细胞分化不完全有关。但FoxM1是如何调节乳腺细胞分化的目前尚不清楚。
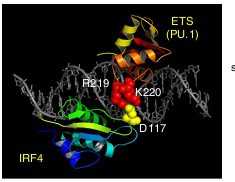
本文的研究者发现,FoxM1以转录抑制因子的身份,来调节管腔上皮祖细胞分化的。在乳腺再生的过程中高表达FoxM1会导致管腔上皮祖细胞数量增多和乳腺导管形态紊乱。与之相反,敲减FoxM1则会导致乳腺细胞的过度分化。研究表明,FoxM1是通过促进GATA3启动子区甲基化,从而抑制GATA-3转录来达到这一效果的。而GATA-3是一个转录因子,其作用正是维持乳腺细胞的导管分化。
这一研究成果说明了FoxM1是调节乳腺细胞分化的关键因子,并为乳腺癌的治疗提供了一个好的靶标。

doi:10.1016/j.celrep.2012.05.005
PMC:
PMID:
FoxM1 Regulates Mammary Luminal Cell Fate
Janai R. Carr, Megan M. Kiefer, Hyun Jung Park, Jing Li, Zebin Wang, Joel Fontanarosa, Danielle DeWaal, Dragana Kopanja, Elizaveta V. Benevolenskaya, Grace Guzman, Pradip Raychaudhuri
Elevated expression of FoxM1 in breast cancer correlates with an undifferentiated tumor phenotype and a negative clinical outcome. However, a role for FoxM1 in regulating mammary differentiation was not known. Here, we identify another function of FoxM1, the ability to act as a transcriptional repressor, which plays an important role in regulating the differentiation of luminal epithelial progenitors. Regeneration of mammary glands with elevated levels of FoxM1 leads to aberrant ductal morphology and expansion of the luminal progenitor pool. Conversely, knockdown of FoxM1 results in a shift toward the differentiated state. FoxM1 mediates these effects by repressing the key regulator of luminal differentiation, GATA-3. Through association with DNMT3b, FoxM1 promotes methylation of the GATA-3 promoter in an Rb-dependent manner. This study identifies FoxM1 as a critical regulator of mammary differentiation with significant implications for the development of aggressive breast cancers.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#CEL#
45
#FOXM1#
43
#Cell#
32