本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
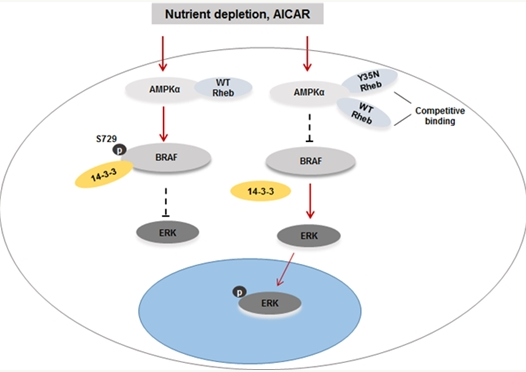
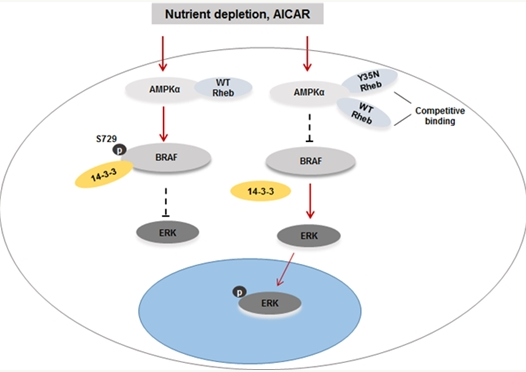

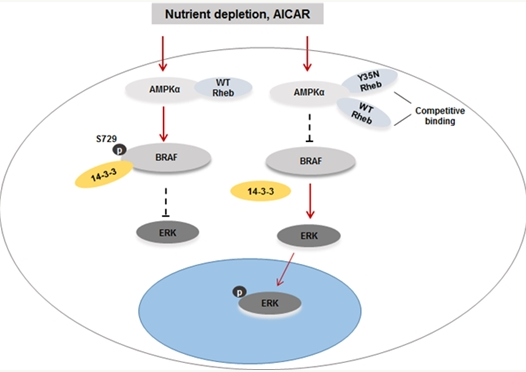
中科院大连化物所生物技术转化医学科学中心刘扬团队在肿瘤转化医学领域取得新进展。该团队首次揭示了Rheb基因突变驱动的肾癌和宫颈癌发生、发展的分子机制,并提供了可潜在用于治疗Rheb突变型肿瘤的新临床策略和方法。相关成果日前发表于《癌基因》杂志。 TSC/mTOR信号通路是调节细胞生存、代谢、增殖和自噬等生物学行为的一条重要信号通路。在很多肿瘤中,该信号通路的异常激活都会导致与肿瘤增殖相关蛋
在一项新的研究中,来自美国斯坦福大学医学院的研究人员发现让肿瘤细胞展示在它们表面上的保护它们自己免受免疫系统吞噬的一种信号也在动脉粥样硬化---经常导致心脏病和中风发作---产生过程中发挥着作用。相关研究结果于2016年7月20日在线发表在Nature期刊上,论文标题为“CD47-blocking antibodies restore phagocytosis and prevent athe
这项发表在Cancer Research杂志上的新近研究指出,通过饮食和锻炼达到减肥目的的肥胖和超重女性血液内参与血管生成相关蛋白质水平降低。 血管生成是指受损血管修复和新血管生成,如果没有氧气和营养物质的供应,机体正常细胞和癌细胞都无法生存。当这些细胞发出相应信号即血管生成因子以促进新血管的生长、癌细胞发展为肿瘤。如果没有血液供应,肿瘤的直径也就几毫米左右。然而,一旦有一些肿瘤细胞分泌相关物质刺
近日,世界权威肿瘤机构——美国德州大学M.D.安德森肿瘤中心将2016年度科研成就奖授予华人肿瘤代谢专家吕志民教授,他也成为该机构本年度肿瘤基础研究领域的唯一获奖者。吕志民现为美国德州大学M.D.安德森肿瘤中心终身教授,多年来一直致力于肿瘤代谢以及相关领域的研究,其团队在肿瘤细胞糖酵解新机制、肿瘤代谢酶与肿瘤发生等领域的独创性研究被认为是国际肿瘤代谢领域的标志性事件,推动了对肿瘤代谢的重新认知,相


梅斯医学MedSci APP
医路相伴,成就大医
#中科院#
33
#Gene#
23
#Oncogene#
43
学习学习!
82