复合型甲状腺发育异常超声表现1例
2019-05-24 闫磊 章建全 曹昆昆 中国医学影像技术
患者女,45岁,发现左侧颌下隆起、颈部不适1月余。超声:左侧甲状腺未见明显甲状腺组织回声(图1A),左侧舌根部可见一类似甲状腺样回声(图1B),范围约13.6mm×8.6mm,边界清,形态似椭圆形;实质回声增粗、减低,分布不均,CDFI见血流信号丰富。左侧颌下见一类似甲状腺样回声(图1B、1C),范围约14.8mm×14.8mm,边界清,形态呈类圆形;实质回声增粗、减低,分布不均,CDFI见点状血
患者女,45岁,发现左侧颌下隆起、颈部不适1月余。超声:左侧甲状腺未见明显甲状腺组织回声(图1A),左侧舌根部可见一类似甲状腺样回声(图1B),范围约13.6mm×8.6mm,边界清,形态似椭圆形;实质回声增粗、减低,分布不均,CDFI见血流信号丰富。左侧颌下见一类似甲状腺样回声(图1B、1C),范围约14.8mm×14.8mm,边界清,形态呈类圆形;实质回声增粗、减低,分布不均,CDFI见点状血流信号。右侧甲状腺大小约12.6mm×5.5mm,实质回声增粗、分布不均匀,CDFI见血流信号丰富。右侧甲状腺旁可见一片状无回声区,内透声好,范围约23.8mm×8.5mm,边界清,形态欠规则。超声诊断:左侧甲状腺缺如,左侧舌根部及左侧颌下异位甲状腺可能;右侧甲状腺明显偏小,考虑发育不全;右侧甲状腺旁囊性结节,淋巴管囊肿可能。
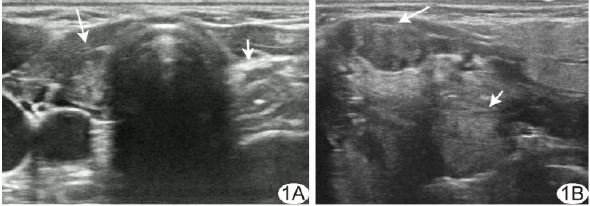
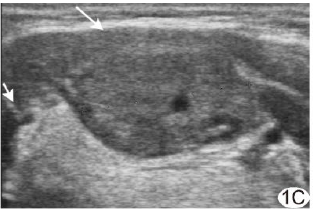
图1 复合型甲状腺发育异常声像图 A.左侧甲状腺区未见明显甲状腺组织回声(短箭),右侧甲状腺体积小(长箭);B.左侧舌根部异位甲状腺(长箭)及左侧颌下异位甲状腺(短箭);C.左侧颌下异位甲状腺(长箭),实质回声增粗、减低,分布不均匀;短箭示左侧颌下腺
实验室检查:T31.28nmol/L,T450.32nmol/L,FT34.01pmol/L,FT47.91pmol/L,超敏促甲状腺激素80.35mIU/L。
SPECT:颈前正中下部见甲状腺右叶显影,体积缩小,放射性分布基本均匀;左叶未显影。左侧颌下及舌根部见放射性团块影。SPECT诊断:右叶甲状腺缩小;左叶甲状腺缺如,舌根部及左侧颌下异位甲状腺(图2)。患者经SPECT明确诊断,给予口服左甲状腺素替代治疗甲状腺功能减退,并定期随访。

图2 SPECT表现 颈前正中下部见甲状腺右叶显影,体积减小,左叶未显影;左侧颌下及舌根部见放射性团块影
讨论
甲状腺发生起始于胚胎发育第3~4周,内胚层细胞增生形成甲状舌管后下降到正常颈部位置,下端膨大发育成甲状腺。甲状腺于胚胎发育过程中如受不良影响可致发育异常,如甲状腺缺如、异位甲状腺及甲状腺发育不全。本例患者为罕见复合型甲状腺发育异常,一侧甲状腺缺如合并同侧两处异位甲状腺,另一侧甲状腺发育不全。
超声为临床常用颈部影像学检查方法,优势为无创、无辐射、简便、价廉、易重复及可实时观察等,可辨别甲状腺的位置、数量、大小及形态结构,有助于甲状腺发育异常的早期诊断。超声检查时如发现甲状腺缺如或发育不全,医师需主动扩大扫查范围寻找是否存在异位甲状腺。甲状腺发育异常多合并甲状腺功能减低,如发现患者其他部位有类似甲状腺回声肿块,需留意颈部是否有正常甲状腺存在,以免误切除异位甲状腺组织,导致永久性甲状腺功能低下。
原始出处:
闫磊,章建全,曹昆昆,吴震中,盛建国,张航.复合型甲状腺发育异常超声表现1例[J].中国医学影像技术,2018,34(03):480.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#超声表现#
42
#发育异常#
41
#发育#
43