Breast Cancer Res:乳腺**处原发癌的激素受体情况可预测对侧乳腺癌风险
2017-07-30 王强 肿瘤资讯
此前已经对乳腺第一处原发癌特征与对侧乳腺癌风险的关系进行了人群基础上的研究;但其中有影响的因素如治疗、乳腺癌家族史、BRCA1/2突变携带情况等信息都未涉及。本文即对乳腺第一原发癌的总体特点、具体特点与对侧非同时发生原发乳腺癌风险的关系进行研究。 患有乳腺癌的女性,对侧乳腺发生第二处原发肿瘤的风险要大于普通女性发生一处原发乳腺癌的风险;且乳腺癌幸存者新发恶性肿瘤中最常见的就是对侧乳腺癌(co
此前已经对乳腺第一处原发癌特征与对侧乳腺癌风险的关系进行了人群基础上的研究;但其中有影响的因素如治疗、乳腺癌家族史、BRCA1/2突变携带情况等信息都未涉及。本文即对乳腺第一原发癌的总体特点、具体特点与对侧非同时发生原发乳腺癌风险的关系进行研究。
患有乳腺癌的女性,对侧乳腺发生第二处原发肿瘤的风险要大于普通女性发生一处原发乳腺癌的风险;且乳腺癌幸存者新发恶性肿瘤中最常见的就是对侧乳腺癌(contralateral breast cancer,CBC)。随着乳腺癌发病率的增加、治疗和预后的改善,乳腺癌患者发生CBC的风险也逐渐增加。此前已经有几项针对乳腺第一原发癌特征与CBC风险间关系的研究,但主要是基于如美国NCI的SEER数据库等癌症注册数据库进行的研究,尽管数据量较大,但一般缺乏重要因素的详细信息,如BRCA1/2突变情况、乳腺癌家族史、第一处乳腺癌治疗情况等。有鉴于此,纪念斯隆-凯特琳癌症中心Reine等人就乳腺第一处原发癌特征与CBC风险方面进行了人群基础上的病例对照研究,相关文章发表于Breast Cancer Research,肿瘤资讯为大家编译介绍如下。
Women’s Environmental Cancer and Radiation Epidemiology(WECARE)研究是一项多中心、人群基础上的病例对照研究,纳入的病例主要有:(1)1985-2008年间确诊为第一处乳腺浸润性癌,但确诊时无局部淋巴结扩散、且首次确诊至少1年后对侧出现了第二处原发的乳腺癌;(2)首次确诊时小于55岁;(3)此前未确诊过相关癌症(非恶性黑色素瘤的皮肤癌或宫颈原位癌除外);(4)随访健在;(5)对该研究知情同意、且愿意提供相关标本;(6)同一癌症注册地区具有上述两种癌症(即第一处乳腺浸润性癌、对侧第二处原发乳腺癌)的其余人群。对侧乳腺完好的对照组也是按照上述纳入标准进行筛选。总计筛选出2354例CBC病例、3599例单侧乳腺癌病例作为对照组,其中1521例CBC、2212例签署了知情同意书并提供了活检材料、完成了随访。通过电话对受试者进行结构性问卷调查,其中涉及已明确或可疑的乳腺癌风险因素,如地域因素、病史、生育史、乳腺癌家族史、激素用药史、吸烟及饮酒情况等;治疗史、肿瘤特点如激素受体情况等则自病理报告与相关医疗文书中提取,同时结合相关数据库进一步提取肿瘤特点相关信息。
数据分析表明,第一处乳腺癌确诊年龄的中位数为46岁,第一处乳腺癌确诊至CBC确诊时间间隔的中位数为6.3年;有75%的受试者首次确诊时未绝经。
第一处乳腺癌为小叶型,则CBC风险增加(风险比RR=1.3),但这一相关性仅限于未应用他莫昔芬者(应用该药者RR=1.0,未应用该药者RR=1.6,异质性P值为0.045)。第一处原发肿瘤的其他特征如分级、分期、淋巴结受累情况、肿瘤大小,均与CBC无相关性。
第一处乳腺癌为激素受体(HR)阴性相比HR阳性来说,CBC风险升高;第一处乳腺癌雌激素受体(ER)阴性相比阳性来说,CBC风险增加30%。雄激素受体(PR)也可见类似趋势:第一处乳腺癌PR阴性相比阳性者CBC风险增加,RR为1.2。ER和PR联合,则第一处乳腺癌ER-/PR-者相比ER+/PR+者的CBC风险升高(RR=1.4)。总体而言,HR状态对CBC风险的影响与是否应用他莫昔芬无关。对进行过HER2检测的受试者进行分析表明,HER2+、三阴表型(ER-/PR-/HER2-)均与CBC风险无显着相关性(二者的RR分别为0.8、1.3)。
对于HR阴性肿瘤而言,第一处浸润性癌确诊后的前10年内,CBC风险的增加最为显着:第一处浸润性癌ER-/PR-相比ER+/PR+者而言,5年内CBC的RR为1.5;≥10年时的RR为1.1。第一处乳腺癌未行他莫昔芬治疗者也有类似结果。一级亲属具有乳腺癌这一家族史(有家族史时,ER-/PR- vs. ER+/PR+的RR为1.5,无家族史时RR为1.3,异质性P值为0.43)、确诊时的年龄(<45岁时ER-/PR- vs. ER+/PR+的RR为1.4,≥45岁时RR为1.3,异质性P值为0.79)并不会影响第一处乳腺癌HR状态与CBC风险间的相关性。
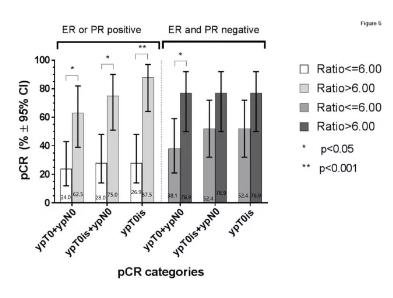
第一处乳腺癌为ER-/PR-相比第一处乳腺癌为ER+/PR+而言,发生ER+/PR+ CBC的可能性更小(RR=0.7);相反,第一处乳腺癌为ER-/PR-者发生ER-/PR- CBC的可能性为第一处乳腺癌ER+/PR+者的五倍(RR=5.4)。第一处乳腺癌确诊时年龄<45岁者RR为5.9,无家族史者RR为5.2,未经他莫昔芬治疗者RR=6.5。
进行过BRCA1/2突变检测的女性中,共计185例为突变携带者(其中109例为病例组、76例为对照组)。除第一处乳腺癌因HR状态不同而导致CBC的RR不同外,第一处乳腺癌为ER-/PR-相比第一处乳腺癌为ER/PR+而言,发生ER-/PR-的CBC风险要高(对全体进行过突变检测的患者来说RR为7.6,对无突变者来说RR为7.7)。将BRCA1有害突变纳入多参数模型时结果也类似(全体进行过突变检测的患者RR为7.6,根据BRCA1有害突变而调整后RR为8.9)。将BRCA1突变携带者排除后,第一处乳腺癌为ER-/PR-、后发生ER-/PR- CBC的风险也类似。
点评
本文从大规模人群基础研究出发,通过病例对照的方式得出结论:第一处乳腺癌的激素受体阴性、组织学类型为小叶型,则发生CBC的风险较高。目前乳腺癌治疗中,激素受体情况已经成为一个重要的参数,因此该研究结果将对患者的预后及风险分层产生重要影响。
原始出处:
Anne S. Reiner, Charles F. Lynch, et al. Hormone receptor status of a first primary breast cancer predicts contralateral breast cancer risk in the WECARE study population. Breast Cancer Research 2017 19:83 https://doi.org/10.1186/s13058-017-0874-x
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#对侧乳腺癌#
34
#乳腺癌风险#
47
#AST#
34
#癌风险#
33
学习了谢谢分享!!
60
#Breast#
36
这个可以有
49
henhao
65
学习了学习了学习了学习了学习了
65
很好,不错,以后会多学习
59