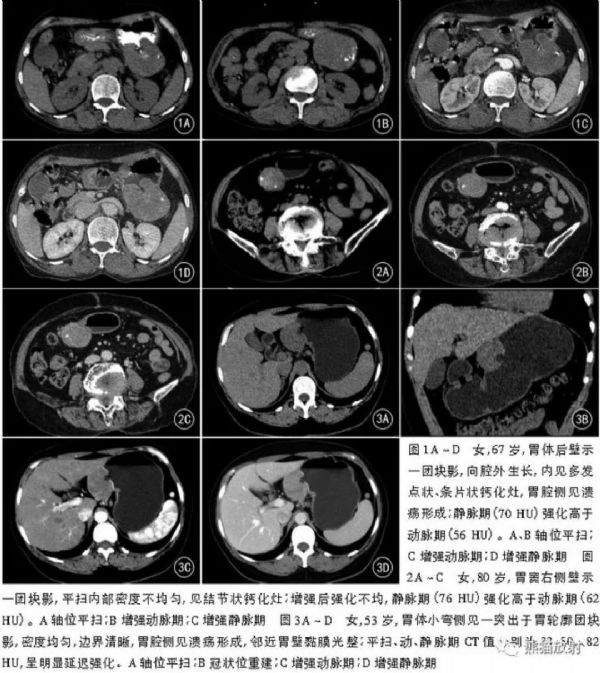
胃间质瘤和胃神经鞘瘤的CT鉴别诊断
2018-07-15 佚名 熊猫放射
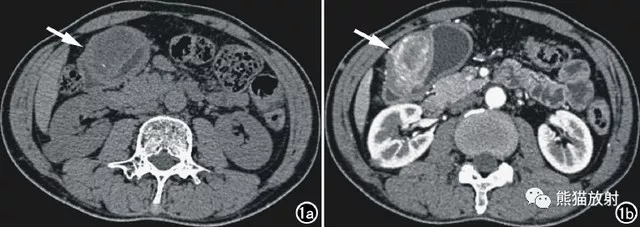
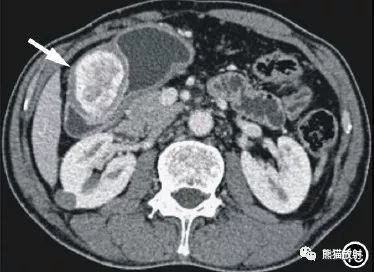
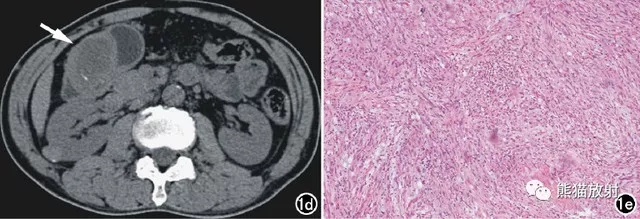
胃窦炎性肌纤维母细胞瘤。男,55岁,黑便3天。a、CT平扫示胃窦部软组织肿块,边界不清,密度不均,中心可见低密度灶,另见小条状钙化灶;b、增强动脉期示病灶边缘明显花环状强化;c、静脉期示对比剂持续填充,呈渐进性不均匀强化;d、未经治疗,第二年病灶的大小、密度、形态均较前无明显变化;e、Ⅱ型梭形细胞密集型(×200,HE)






本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


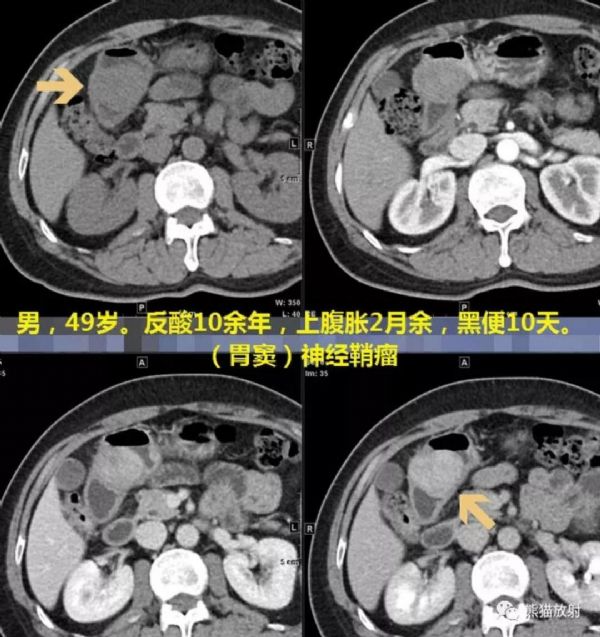
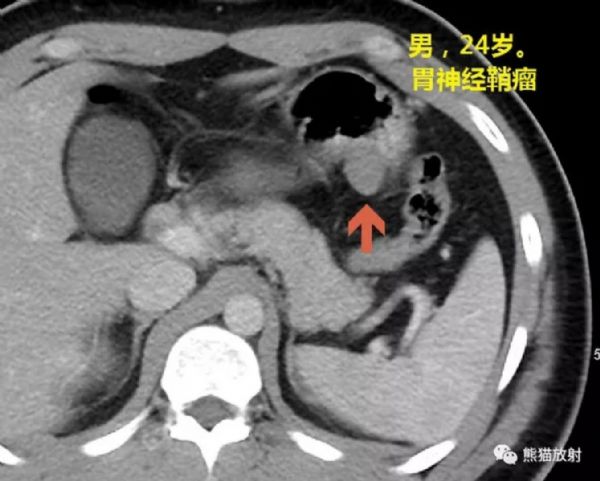
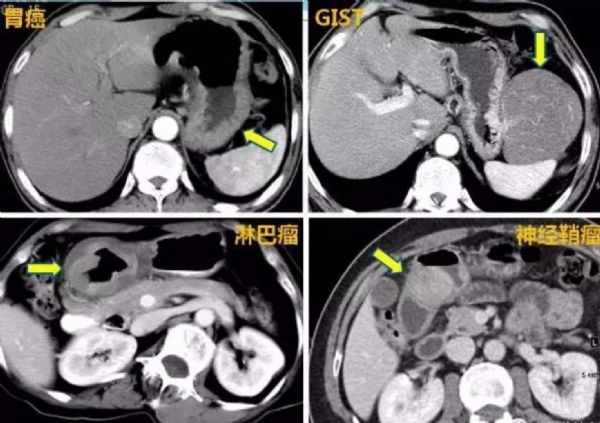








#神经鞘瘤#
37
#间质瘤#
39
#鉴别诊断#
50
#胃间质瘤#
56
不错
75
学习了.谢谢分享.
1