【一般资料】
女,57岁;
【主诉】
因“间断发作性肢体抽搐1年”于2015年10月10日入院
【现病史】
平均每周发病3~5次,每次持续约1min,不伴意识障碍。
【体格检查】
一般状况好,神志清楚,言语流利。
【辅助检查】
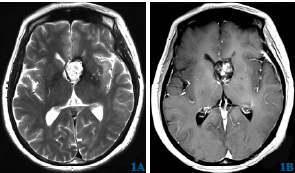
长程视频脑电图示:异常脑电图及脑电地形图。头部MRI示:第三脑室前部、左侧侧脑室前角与相邻脑室旁可见片状不均质信号占位。静脉注射对比剂后,病变呈斑片状不均质强化,延迟扫描强化程度略增高,大小约3.4cm×2.5cm×2.1cm。
【初步诊断】
考虑海绵状血管瘤。
【治疗】
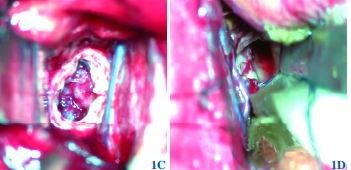
于2015年10月25日行手术治疗。手术采用经纵裂-胼胝体入路,在纵裂侧牵开额叶,沿大脑镰向深部探查,纵行切开胼胝体,进入侧脑室释放脑脊液后可见葡萄串珠样肿物,呈灰红色,血运丰富,分块切除肿瘤,可见肿瘤血供来自脉络丛血管,予镜下全切除肿瘤。病理报告诊断为:海绵状血管瘤伴出血。术后复查MRI示病变全切除,病人肢体抽搐症状完全缓解。随访1年,头部MRI复查无复发,无新增症状。
【讨论】
海绵状血管瘤是一种可以生长在中枢神经系统任何部位的血管错构瘤。近年来,由于计算机层析成像及MRI普及,海绵状血管瘤的诊断率越来越高。脑室内海绵状血管瘤仅占所有颅内海绵状血管瘤的2.5%~10.8%。脑室内海绵状血管瘤最常发生于侧脑室,生长在第三脑室的海绵状血管瘤相当罕见。第三脑室肿瘤周围脑组织缺乏,肿瘤生长阻力较低,脑室内海绵状血管瘤生长速度较快,可形成巨型畸形。因此,由占位效应所引起的临床症状的发生率较高。本例病人以间断发作性肢体抽搐起病,结合其脑电图及MRI表现,本组认为是脑室内海绵状血管瘤反复出血引起的癫疒间发作。第三脑室内海绵状血管瘤与颅咽管瘤、生殖细胞瘤等第三脑室占位性病变难以鉴别,影像学表现对其诊断及后续治疗非常重要。海绵状血管瘤在MRI表现为:在T1和T2加权像上,中央区高铁血红蛋白相关的高信号影,而周边钙化纤维化区域低信号影。另外,肿瘤组织呈“充填式”强化有助于本病的诊断。本例病人MRI上在T1WI和T2WI上均呈混杂信号,可能是近期肿瘤出血所致,与文献所述一致。幕上无症状海绵状血管瘤更适合保守治疗,但第三脑室海绵状血管瘤生长迅速,易出血,位置与许多重要结构相连,且海绵状血管瘤可以通过完整切除治愈,故应获得更积极的治疗方案。生长在第三脑室的海绵状血管瘤,最好选择短途手术入路,以观察到出血引起病变的表面改变,便于分离及切除肿瘤。考虑这些因素,经纵裂-胼胝体入路是最直接、短途的第三脑室病变全暴露的手术方式。本例第三脑室内海绵状血管瘤较大,并侵犯下丘脑,手术过程中应避免损害下丘脑。减少这一并发症的关键是最大限度减少切除含铁血黄素染色组织,并保留相关发育性静脉畸形。另外,本例术中可见肿瘤血供来自脉络丛血管。有文献表明对第三脑室海绵状血管瘤病人行DSA检查可见扩大的脉络膜动脉引起肿瘤充血现象。因此,脑室内海绵状血管瘤的切除中,应仔细探查肿瘤与脉络膜动脉及其分支的联系,电凝肿瘤供血动脉可使肿瘤丧失血供软化坏死,还可减少术中出血,提高肿瘤全切除率。若术中出血较多,肿瘤切除难度较大时,可部分切除,明确海绵状血管瘤的病理诊断后,辅以立体定向或伽玛刀治疗,可得到较好的治疗效果,同时可以避免发生并发症。

版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#脑室内#
32
#血管瘤#
30
#海绵状血管瘤#
32
#海绵状#
23
#脑室#
35
牛
45
谢谢病例分享.学习了.
40