Cell Host & Microbe:肠道菌群失衡和衰老如何相互加剧?
2017-04-20 杜焱恭 学术经纬
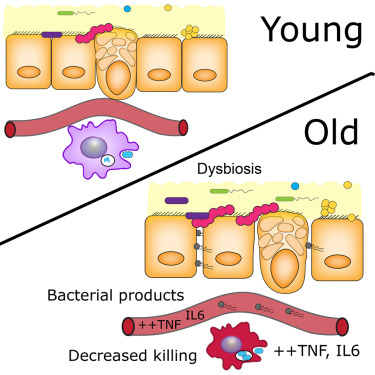
最近,加拿大麦克马斯特大学(McMaster University)的科学家们发现,肠道微生物在小鼠体内可引起衰老相关炎症和过早死亡。老年小鼠肠道微生物组成失衡(dysbiosis)可能导致肠道渗漏,向体内释放引发炎症的细菌产物,进而损害免疫功能和减少寿命。这项发表在《细胞》子刊《Cell Host & Microbe》研究可能提示改善老年人肠道健康和免疫功能的新策略。其实,类似的现象已在

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Micro#
33
#CEL#
33
#Cell#
33
#CRO#
33
#肠道菌#
39
非常好的研究学,习了,很受益。
65