PLoS Biol:重磅!抗生素耐药性产生新方式
2016-12-31 佚名 生物谷
在一项新的研究中,来自荷兰格罗宁根大学和美国加州大学圣地亚哥分校的研究人员发现对抗生素敏感的细菌当它们的周围有足够多的耐药性细胞表达一种抗生素灭活因子时,也能够存活下来。相关研究结果于2016年12月27日发表在PLoS Biology期刊上,论文标题为“Collective Resistance in Microbial Communities by Intracellular Antibiot
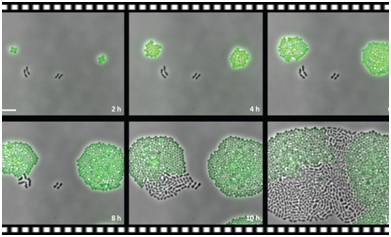
研究人员观察到已被绿色荧光蛋白(GFP)标记的葡萄球菌表达一种氯霉素耐药性基因。在它们附近的是黑色的没有携带这种耐药性基因的肺炎链球菌。在一种含有氯霉素的培养基中,发出绿色荧光的葡萄球菌开始生长和发生分裂,然而非耐药性的黑色的肺炎链球菌则不会。在一段时间后,单个黑色的肺炎链球菌开始发生分裂,而且它们甚至在生长上超过发出绿色荧光的葡萄球菌。
论文第一作者、格罗宁根大学合成生物学中心微生物学家Robin Sorg解释道,“这些耐药性的细胞摄取氯霉素,而且让它失活。在某个时间点上,培养基中的氯霉素浓度下降到一种临界水平下,因而非耐药性的细胞开始生长。”类似的事情也在之前观察过。“对青霉素产生耐药性的细胞能够分泌降解这种抗生素的β-内酰胺酶。但是在我们的研究中,抗生素是在耐药性的细胞中被灭活的。”
延时摄影
这一发现是利用时差显微镜取得的,而且利用计算建模和一种小鼠肺炎模型加以证实。“在小鼠体内,我们观察到当这些小鼠同时感染上耐药性细菌时,敏感的肺炎链球菌在接受氯霉素治疗后能够存活下来。”再者,这些结果排除了耐药性基因转移的情形。
因此,当耐药性的细菌存在时,敏感的细菌能够存活更长的时间,而且最终甚至能够竞争得过它们。对抗生素耐药性扩散来说,这意味着什么?Sorg说,“它是复杂的。我们知道抗生素使用导致耐药性选择。然而,我们并没有充分地理解着这些过程和抗生素耐药性为何如此快速地产生。类似我们的研究的单细胞研究有助填充其中的一些细节。”
代谢
一件应当值得注意的事情是这项实验中,这些敏感的细胞停止生长,但是不会死亡。“很多抗生素诱导的杀死机制依赖于发生分裂的细胞,或者至少依赖于发生活跃代谢的细胞。”不杀死这些敏感的细胞可能不会让它们变得更加强大,但是当然会给它们从它们的环境中获取耐药性基因的时间。
当利用抗生素治疗病人时,这种知识能够有助于医生。“我们知道我们应当慎重地使用这些药物,但是我们可能需要比我们所认为的更加谨慎。”Sorg概述了一种个人化治疗方法:存在于病人体内的非致病性细菌应当接受耐药性基因检查。“这会增加[耐药性基因]转移到病原菌中的风险。”
为了阻止非致病性微生物产生耐药性,尽可能少地使用抗生素当然是比较重要的。可能有朝一日,当对负责抗生素耐药性扩散的机制的理解更加完整时,人们就可能找到一种阻止它的方法。
Robin A. Sorg, Leo Lin, G. Sander van Doorn, Moritz Sorg, Joshua Olson, Victor Nizet, Jan-Willem Veening.Collective Resistance in Microbial Communities by Intracellular Antibiotic Deactivation.PLoS Biol.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Biol#
33
#新方式#
37
#Bio#
35
这个有很大意义
62
#抗生素耐药#
39
#重磅#
27
#抗生素耐药性#
30
抗生素滥用已成为人类未来最大的威胁之一
50