Nature:临床研究私人定制时代来临
2015-05-12 孙学军 孙学军博客
许多人每天吃药,可是这些药物对具体个人会产生多大好处,许多人可能并不了解。从整体上考虑,吃药物能得到效果的比例从4%到25%不等。这也正是精准医疗如此受人追捧的重要原因,因为人们都希望能找到针对每个人能产生效果的治疗方法和药物。解决这一问题的办法就是要将每个人作为一个独特的个体,根据这一思想建立的研究策略就是个性化临床研究。国际上称为N of 1,就是样本数为1的研究。 成千
许多人每天吃药,可是这些药物对具体个人会产生多大好处,许多人可能并不了解。从整体上考虑,吃药物能得到效果的比例从4%到25%不等。这也正是精准医疗如此受人追捧的重要原因,因为人们都希望能找到针对每个人能产生效果的治疗方法和药物。解决这一问题的办法就是要将每个人作为一个独特的个体,根据这一思想建立的研究策略就是个性化临床研究。国际上称为N of 1,就是样本数为1的研究。
精准医疗的基础是每人都是独特的,这也是让大家立刻赞成的重要原因。2015年1月美国总统奥巴马宣布投入2.15亿美元投入精准医疗,其中包括建立100万美国人规模的基因等相关数据库。
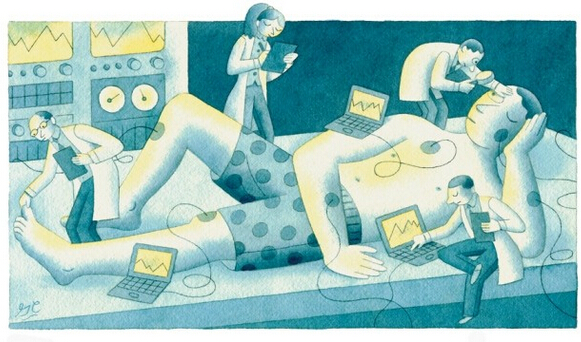
传统的临床研究是对数***进行检测分析,精准医疗需要不同的检测方法和干预措施。科学家需要调查多种因素,包括遗传、环境和其他因素,这些因素都会对患者治疗相应产生影响。
针对个体的研究将对解决许多问题产生帮助,从某种意义上讲,过去医生也一直采用类似策略,例如心内科医生给高血压患者开药后,会根据该药对血压控制的效果来确定是否更换其他药物。但是很少有医生和科学家会将这种方法变成周密设计的研究方案,如果分析检测的指标很多,对个人治疗评估也可以按照研究来进行。
如果数据采集时间足够长,采集到的数据量足够多,使用适当的对照,那么一个个体可以作为某一治疗是否有响应的研究。对这些个体实验结果进行汇总可获得某一治疗对人群的效应。这是一种将群体研究化整为零的概念,将对临床研究的快速发展产生促进作用。
个体化临床研究广泛使用还需要解决许多具体问题,如需要开发更好的健康监护新设备,确定更准确的疾病生物标记物,如血液中肿瘤DNA,也需要监管机构、制药公司和临床医生等各个层面都在文化和理念上的转变。
研究发现,对某一特定群体的疾病效果治疗有效的机会经常比较偶然,在后期的大规模人群药物研究中结果通常会令人失望,这一问题促使科学家在研究结束后,试图通过个体专门分析确定影响效果的人群因素,以挽救失败的研究。
传统的三期临床需要数千名患者,治疗和干预手段需要随机分组,一组进行干预治疗,另一组给予安慰剂糖丸假治疗对照。这种研究一般不收集遗传、饮食和生活方式等因素的数据,许多试验结果发现,应该根据有效性本身对患者进行分层研究,或者说受试对象本身存在干扰研究结果的问题,有些患者根本就应该被排除在外。
一些试验设计试图对患者进行分类,例如针对癌症的Basket trials,就是根据作用模式和疾病种类检测干预有效性。2015年5月将启动的美国癌症研究院MATCH Trial根据1000名晚期癌症患者的基因标志类型,分成不同治疗的baskets。每个Baskets包括30名左右患者,每组患者存在共同的基因异常类型,将从25种药物种选择一种给于治疗。研究最终确定出不同基因异常对应的有效治疗药物。
雨伞型试验中,科学家将研究多种药物对一种疾病治疗的有效性,这种研究模式将被癌症和黑色素瘤研究联盟梦之队进行临床试验中采用。耶鲁大学和转化基因组研究院共同负责这一项目。试验将对100名晚期黑色素瘤患者中的70名根据基因组数据选择治疗方法,从40种药物中匹配药物,其余患者将采用标准治疗方法。研究最终确定出那些药物对相应基因异常的治疗最理想。
虽然这些试验设计仍不够个体化,虽然某一突变能被特定药物治疗,但是患者效应还会受到许多非基因因素影响。例如威罗菲尼是FDA授权治疗晚期黑色素瘤携带BRAF突变患者的药物。但一些肿瘤细胞能产生对抗这种药物的其他变异。
个体化临床研究时,患者个人的所有相关数据都将被收集,收集次数尽可能多,如每天、每月或每年。一些研究设计、统计学技术仍可以采用,例如患者和医生对检测药物的双盲,使用对照干预等。适当交叉设计(自身对照),就是分析同一受试者对干预的不同阶段进行比较,一般可设置药物清洗期与使用期进行比较。
统计分析过去主要为群体研究服务,但如果适当改进,针对个人对单个干预也可以使用统计分析。在澳大利亚的一项研究中,对132名骨关节炎和慢性疼痛患者3年内使用不同药物治疗效果的评价,评价指标包括疼痛水平、组织水肿和其他相关症状。这里要注意的是,研究对象是132名,不是很大的样本量,分析多种药物的效果差异。如果按照经典的双盲随机对照,这几乎是不可能实现的目标,但采用N-of-1trials(个体化临床研究)就不同了。因为这种方法是对每个患者进行每2周持续12周的反复检测,这期间包括患者服用和停止服用某种药物。通过对不同药物服用前后数据进行比较,研究人员发现,虽然费用增加,但对优化处方的效率提高了。
但是也不能神话个体化临床研究,这种方法对有些问题的解决并没有帮助。关于公共卫生方面的研究就很难使用这种方法,例如饮用水添加氟。饮用水添加氟与肿瘤发生的关系就很难使用这种方法。但是在许多情况下,个体化临床研究是一种理想的方法。尤其是对一些罕见病的研究,因为发病人数很少,根本没有办法进行传统的随机双盲对照研究。如果要验证药物的效果,就只能采用这种研究方法。临床实践中,一些仍然处于研究中的药物因为“同情”因素被用于患者,更多医生给无药可用的患者使用非标治疗药物。例如用美西律治疗肌强直和埃博拉病毒的实验治疗等。
精心设计的N-of-1试验也可用于临床药物开发早期阶段或老药新用的研究。I和II期临床试验通常需要给一小群健康志愿者不同剂量药物,那么准确估计某一药物适当的安全剂量就可以使用N-of-1方法。
N-of-1试验也能指导临床工作,如确定疾病的发生。例如,美国医生通过分析血液中CA125蛋白水平超过30-35作为卵巢癌的筛选指标,但是如果患者过去8年这一蛋白水平只有10-15,那么只要增加到20-25(相当于增加一倍),就应该引起重视。个性化诊断需要对每个人建立各种数据的历史资料。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Nat#
27
这篇文章有一定深度
104
是一篇不错的文章
116
学习,总结
111
嗯嗯
132
看看
161
日积月累,你会越来越棒
91
自己认为的可以不是真的可以,要学会聪明
56
大多数药物研究都是基于西方人群进行的临床研究。
84
学习了,很好
80