【病史临床】
男,56岁,右耳反复流脓2年余,加重伴听力下降、疼痛2月,突发右侧周围性面瘫3周。
【影像图片】
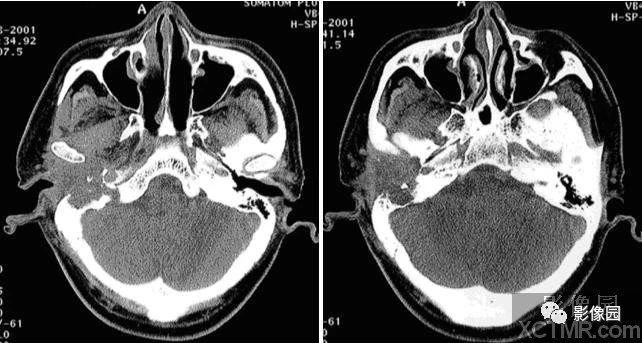
平扫A 平扫B
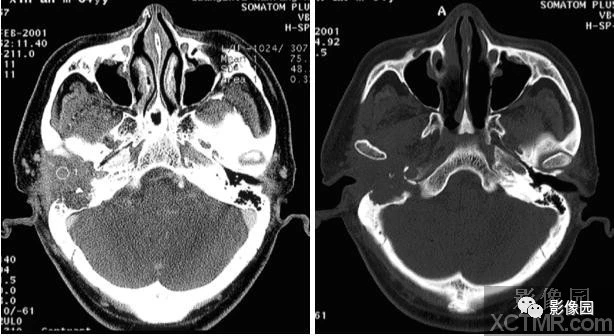
增强D 骨窗E

增强C
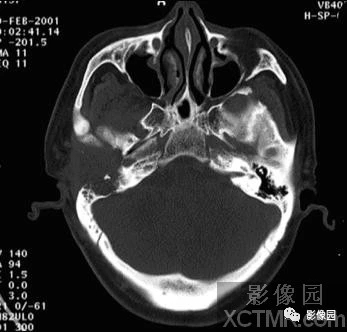
骨窗F
【影像表现】
横断面平扫(A、B)示右侧外耳道、中耳区见软组织肿块影,大小约3.9×3.8cm;增强扫描(C、D)示肿块有强化,向前侵犯右侧颞骨鳞部,向外侵犯右侧腮腺,向内、后侵犯颞骨岩部、乳突;骨窗(E、F)示外耳道、中耳、乳突骨质不规则虫蚀状破坏。
【诊断】
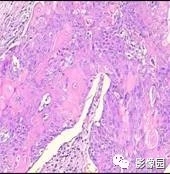
右耳高-中分化鳞状细胞癌 (病理确诊)送检组织可见瘤细胞呈片巢状或团块状分布,细胞大小不一,细胞连接紧密,可见细胞间桥,胞浆红染,可见细胞内角化,细胞核形态不规则,胞核深染,核膜清晰,核仁明显。
【鉴别诊断】
胆脂瘤型中耳炎
【讨论】
中耳癌(carcinoma of middle ear)占全身癌的0.06%,占耳部肿瘤的5%~10%。病理类型以鳞癌多见。临床表现早期症状少,易出血,可有脓性耳漏,耳内闷胀感、耳鸣与听力减退,因伴中耳炎常被忽视。
影像诊断要点及鉴别诊断:(1)高分辨率CT上能清楚显示外耳及中耳骨质结构不规则及多点虫蚀状破坏,破坏骨质无硬化边。(2)增强扫描强化明显,可与胆脂瘤相鉴别。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#细胞癌#
29
#CT病例#
31
学习了!!!!!!
0