AASLD2017:定量抗-HBc水平可预测慢乙肝停药后复发风险
2017-10-22 佚名 国际肝病
部分符合条件的慢性乙型肝炎(CHB)患者或许可以尝试停用核苷(酸)类似物(NA)治疗,然而,尚无客观一致的指标用于预测患者停药后的持续应答。最近,有研究表明,定量抗-HBc水平可以预测CHB患者对NA以及干扰素治疗的应答。那么,定量抗-HBc水平是否也可能在预测停药后复发风险上发挥用武之地呢?
部分符合条件的慢性乙型肝炎(CHB)患者或许可以尝试停用核苷(酸)类似物(NA)治疗,然而,尚无客观一致的指标用于预测患者停药后的持续应答。最近,有研究表明,定量抗-HBc水平可以预测CHB患者对NA以及干扰素治疗的应答。那么,定量抗-HBc水平是否也可能在预测停药后复发风险上发挥用武之地呢?
当地10月21日,来自荷兰鹿特丹伊拉斯谟大学医学中心的Heng Chi在2017年第68届美国肝病协会年会(AASLD)上给出了支持证据。他们的最新研究结果显示:定量抗-HBc水平可以准确预测CHB患者停用NA后的复发风险,有望用于选择可以停止NA治疗的患者。
该项前瞻性研究对停用NA、无肝硬化的亚裔CHB患者进行随访,停药前HBeAg阳性患者已经获得HBeAg血清学转换和HBV DNA检测不出,并且进行巩固治疗≥12个月,HBeAg阴性患者要求达到HBV DNA检测不出≥18个月。最初3个月,每1个月对患者进行随访,然后,每3个月进行随访。对HBV DNA >2000 IU/mL且ALT >2倍正常值上限(临床复发)的患者进行再治疗。应用双抗夹心定量免疫方法检测患者的血清抗-HBc水平,对其用于预测患者停用NA后复发风险的价值进行评估。
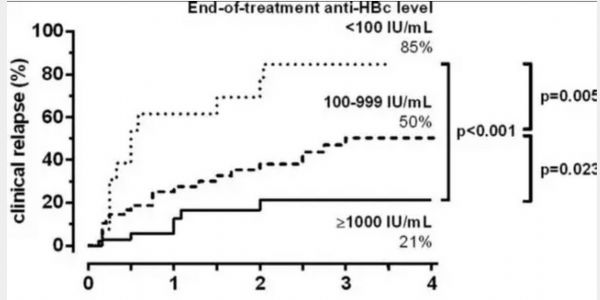
结果,对100例患者(开始NA治疗时,71%为HBeAg阳性,平均年龄为35岁,86%为男性)进行随访的中数时间为2.5年,39例患者发生临床复发,4年时的临床复发率为46%。对年龄、开始NA治疗时的HBeAg阳性状态以及巩固治疗时间进行校正后的模型分析表明,停止治疗时抗-HBc水平较高(每增加1 log IU/mL的HR:0.31,P=0.002)和停止治疗时的HBsAg水平较低(每增加1 log IU/mL的HR:1.71,P=0.032)与临床复发的风险降低有关,详见下图。
停止治疗时的HBsAg水平≤100 IU/mL也与持续应答有关(HR:0.30,P=0.045),然而许多患者(82%)停止治疗时的HBsAg水平>100 IU/mL,应用这些患者停止治疗时的抗-HBc水平可以对复发风险进一步分层(每增加1 log IU/mL的HR:0.39,P=0.005)。临床复发的患者与维持应答的患者相比,停止治疗时的抗-HBc水平升高更加急剧(+3.6对比+0.5 log IU/mL/年,P<0.001)。停止治疗后4周、8周、12周和24周时的抗-HBc水平变化并不能预测将来的复发风险(所有P值均>0.05)。
原始出处:
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#复发风险#
28
#AASLD#
26
#停药#
27
#ASL#
36
谢谢分享.学习了
60
谢谢.学习了.很好
54