European Radiology:如何实现低剂量MRA的动静脉畸形显影?
2022-07-24 shaosai MedSci原创
现阶段,使用钆剂(GBCA)的动态增强磁共振血管成像已被认为是替代DSA的一种无创成像方法。
 常规数字减影血管造影(DSA)由于其高空间和时间分辨率,是诊断颅内和颅外血管病变的金标准,是评估包括动静脉畸形(AVM)和动静脉瘘(AVF)在内的动静脉分流(AVS)最重要的成像方式之一。然而,由于DSA有神经系统并发症的风险,并且在手术过程中需要暴露于电离辐射,因此并不适合用于随访观察或筛查。
常规数字减影血管造影(DSA)由于其高空间和时间分辨率,是诊断颅内和颅外血管病变的金标准,是评估包括动静脉畸形(AVM)和动静脉瘘(AVF)在内的动静脉分流(AVS)最重要的成像方式之一。然而,由于DSA有神经系统并发症的风险,并且在手术过程中需要暴露于电离辐射,因此并不适合用于随访观察或筛查。
现阶段,使用钆剂(GBCA)的动态增强磁共振血管成像已被认为是替代DSA的一种无创成像方法。最近的研究表明,采用迭代重建的TWIST(IT-TWIST)改善了微血管的可视化程度。由于对GBCA在人体内蓄积的安全担忧,使用低剂量GBCA TWIST-MRA与迭代重建(以下简称IT-TWIST-MRA)可实现对AVS的准确识别。据我们所知,尚未有研究使用IT-TWIST-MRA评估全脑和颈部AVS的效用,以及IT-TWIST-MRA与其他成像方式(如DSA)之间的一致性。
近日,发表在European Radiology杂志的一项研究评估了IT-TWIST-MRA与低剂量GBCA作为头颈部的4D MR-DSA的技术可行性,并比较了IT-TWIST-MRA在评估AVS时的诊断性能,为临床选择筛查及随访手段提供了新的选择及参考。
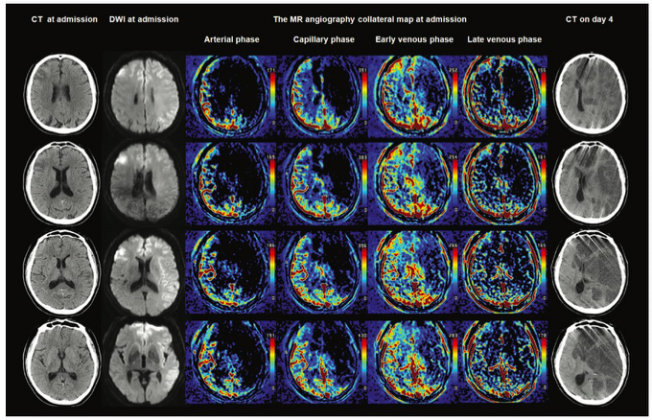
本项研究在2016年9月至2019年10月期间对29名已知AVS患者在3-T MRI扫描仪上进行了TWIST-MRA检查,使用低剂量注射钆造影剂(GBCA),并进行了傅里叶和迭代重建。对图像质量进行了视觉评估,以划定(a)正常的脑动脉和静脉以及(b)AVS的供血、分流和引流血管。进行兴趣区评估,以评价脑血管信号强度的栓塞清晰度和基线信号的波动,并比较了TWIST-MRA和IT-TWIST-MRA对AVS的检测。采用配对样本Wilcoxon检验来检验TWIST-MRA和IT-TWIST-MRA之间的差异。
使用IT-TWIST-MRA重建的图像对正常血管和AVS血管结构的可视化评分明显优于使用TWIST-MRA的图像。除上矢状窦(SSS)外,IT-TWIST-MRA的峰值信号和时间强度曲线的增强斜率都明显高于TWIST-MRA。除SSS外,IT-TWIST-MRA的基线强度波动明显低于TWIST。
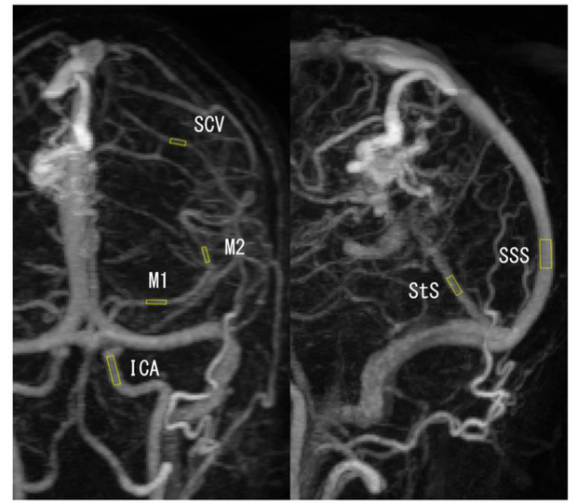
图 用于定量分析的兴趣区域安置.ICA,颈内动脉;M1,大脑中动脉(MCA)的M1部分;M2,MCA的M2部分;SSS,上矢状窦;StS,直窦;SCV,大脑浅静脉
本研究表明,迭代重建产生的4D MR-DSA图像可满足临床实践中的对图像的要求,即使使用低剂量的GBCA也能清晰显示AVS,因此IT-TWIST-MRA可成为传统DSA和MRI评估和监测AVS的一个有用的辅助成像选择。
原文出处:
Akihiko Sakata,Ryo Sakamoto,Yasutaka Fushimi,et al.Low-dose contrast-enhanced time-resolved angiography with stochastic trajectories with iterative reconstruction (IT-TWIST-MRA) in brain arteriovenous shunt.DOI:10.1007/s00330-022-08678-7
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#动静脉畸形#
29
#静脉#
69
#PE#
41
#畸形#
43
#低剂量#
36
#MRA#
35