JACC:替卡格雷治疗糖尿病患者,降低缺血事件发生
2016-05-19 phylis 译 MedSci原创
背景:糖尿病患者与动脉粥样硬化事件发生的风险升高相关。目标:确定对存在心肌梗死病史(MI)的糖尿病患者,应用替卡格雷抗血小板治疗对复发性缺血事件的影响。方法:研究者将PEGASUS-TIMI 54试验中患者分为,糖尿病患者(n = 6806)和非糖尿病(n = 14355)患者两个亚组,其中21162例患者1-3年的心肌梗死史与其他危险因素的患者随机分为替卡格雷(90毫克或60毫克/每日两次)或安
背景:糖尿病患者与动脉粥样硬化事件发生的风险升高相关。
目标:确定对存在心肌梗死病史(MI)的糖尿病患者来说,应用替卡格雷抗血小板治疗对复发性缺血事件的影响。
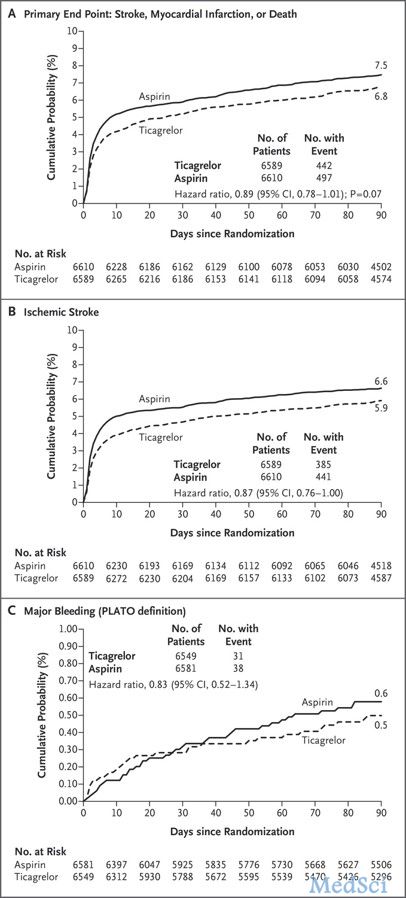
方法:研究者将PEGASUS-TIMI 54试验中患者分为,糖尿病患者(n = 6806)和非糖尿病(n = 14355)患者两个亚组,其中21162例患者1-3年的心肌梗死史与其他危险因素的患者随机分为替卡格雷(90毫克或60毫克/每日两次)或安慰剂组治疗。随访中位数为33个月。主要疗效终点为主要不良心血管事件(MACE:心血管死亡、MI、卒中)和主要安全性终点是TIMI主要出血。
结果:与安慰剂相比组,替卡格雷治疗的糖尿病患者(HR 0.84 95% CI 0.72-0.99)和糖尿病患者(HR 0.84,95% CI 0.74-0.96),MACE发生的相对风险降低是一致的。因为糖尿病患者发生MACE的风险更高,与非糖尿病患者相比,糖尿病患者绝对风险降低(APP)较高(1.5% vs 1.1%,相应的NNT3年为67 vs 91)。需要药物治疗的糖尿病患者(n = 5960),ARR为1.9%和NNT3年53。此外,替卡格雷治疗的糖尿病患者,心血管死亡降低22%(HR 0.78;95% CI 0.61-0.99)和冠心病死亡下降34%(HR 0.66,95% CI 0.48-0.91,P = 0.01)。与非糖尿病患者一致,糖尿病患者TIMI主要出血增加:HR 2.56,95% CI 1.52-4.33。
结论:存在心肌梗死史的糖尿病患者,替卡格雷联合阿司匹林显著降低复发性缺血事件的风险,包括心血管疾病和冠状动脉心脏病死亡。
原始出处:
Bhatt DL, Bonaca MP, et al. Reduction in Ischemic Events with Ticagrelor in Diabetic Patients: From the PEGASUS-TIMI 54 Trial. J Am Coll Cardiol. 2016 Mar 30.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#JACC#
19
#ACC#
32
#替卡格雷#
34
#糖尿病患者#
32