JACC:阿哌沙班不能改善ACS患者预后
2015-08-17 徐媛媛 MedSci原创
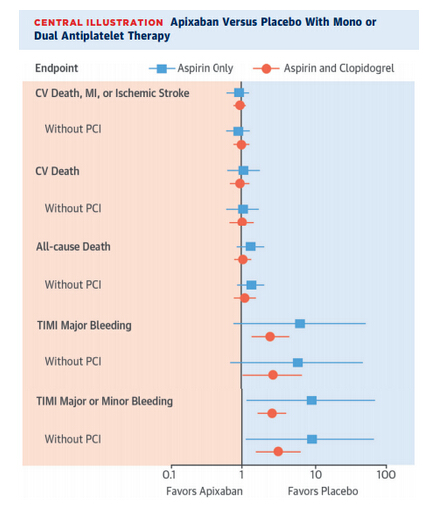
APPRAISE-2研究最新发现表明,无论ACS患者使用阿哌沙班时是否联合抗血小板治疗,阿哌沙班都不能改善其预后,而且会增加出血风险,该试验也因此被提前终止。阿哌沙班未改善ACS患者预后Connie N. Hess(杜科临床研究所)称,研究者对阿哌沙班疗效是否受到抗血小板治疗(阿司匹林或阿司匹林加氯吡格雷)影响进行了分析。基线时,7364例患者中16.3%在服用阿司匹林,79%在联用阿司匹林与氯吡
出血限制了对急性冠脉综合征(ACS)患者的抗凝治疗。本文对阿哌沙班疗效是否受到抗血小板治疗影响进行了分析。
本研究评估了高风险ACS患者接受阿司匹林或阿司匹林+氯吡格雷和接受安慰剂ACS患者。在因果分析中,研究人员评估阿哌沙班是否可改善ACS患者预后或减少出血风险。
研究结果,基线时,7364例患者中有16.3% (n=1,202) 服用阿司匹林,79% (n=5,814) 在联用阿司匹林与氯吡格雷;随访过程中,19.2%(n=1,415)转为抗血小板治疗。研究人员对患者的复合终点(心血管死亡、心梗及缺血性卒中)进行了评估,结果发现无论患者是否在服用阿司匹林(阿哌沙班 12.21/100人年,安慰剂 13.21/100人年;校正HR = 0.91;95% CI,0.62-1.32)或阿司匹林加氯吡格雷阿哌沙班(阿哌沙班 13.22/100人年,安慰剂 14.24/100人年;校正HR = 0.95;95% CI,0.78-1.14;P=0.84),阿哌沙班与安慰剂的疗效并无差异。无论患者是否使用阿司匹林(阿哌沙班 1.48/100人年,安慰剂 0.25/100人年;校正HR = 6.62;95% CI,0.75-51.73)或阿司匹林加氯吡格雷(阿哌沙班 2.58/100人年,安慰剂 1.02/100人年;校正HR = 2.44;95% CI,1.34-4.45;P=0.41)。
研究结果表明,无论ACS患者使用阿哌沙班时是否联合抗血小板治疗,阿哌沙班都不能改善其预后,而且会增加出血风险,该试验也因此被提前终止。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#患者预后#
27
#JACC#
29
好好去看看
131
#ACS#
24
#ACC#
23
#ACS患者#
34
有点用
79