Lung Cancer:PET/CT评价肺癌纵膈淋巴结转移作用有限
2014-05-22 佚名 dxy
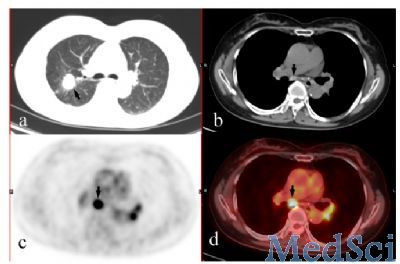
肺腺癌和鳞癌是最常见的非小细胞肺癌,对其的合理治疗需要准确的临床分期。纵膈镜检查目前仍被认为是确定纵膈淋巴结状态的金标准,但很多发展中国家并未常规性进行该项检查。非侵入性检查方法中,CT检查因主要基于淋巴结大小不够精确。18F-FDG PET/CT检查对于评价直径<15mm的淋巴结可能具有一定意义。 针对这种情况,中国哈医大肿瘤医院的Yu医生等进行了一项回顾性研究,发现18F-FDG PE
肺腺癌和鳞癌是最常见的非小细胞肺癌,对其的合理治疗需要准确的临床分期。纵膈镜检查目前仍被认为是确定纵膈淋巴结状态的金标准,但很多发展中国家并未常规性进行该项检查。非侵入性检查方法中,CT检查因主要基于淋巴结大小不够精确。18F-FDG PET/CT检查对于评价直径<15mm的淋巴结可能具有一定意义。【原文下载】
针对这种情况,中国哈医大肿瘤医院的Yu医生等进行了一项回顾性研究,发现18F-FDG PET/CT对腺/鳞癌直径<15mm的淋巴结的评价作用有限,且在鳞癌中假阳性率较高,考虑CT的衰减性有助于提高准确性。文章发表在2014年5月的Lung Cancer上。
该回顾性研究纳入了2005年10月至2012年10月间术前接受18F-FDG PET/CT检查且伴有直径<15mm纵膈淋巴结的116例腺癌和234例鳞癌患者,所有患者随后进行了病理检查确诊,对比PET/CT与病理检查结果间的差异。
研究结果显示,PET/CT检查在腺癌组中的特异性和准确性较鳞癌组高。与PET相比,PET/CT对鳞癌组有着更高的特异性和准确性,对腺癌组有着更高的特异性、准确性和阳性预测值。
原始出处
Lu P1, Sun Y2, Sun Y1, Yu L3.The role of 18F-FDG PET/CT for evaluation of metastatic mediastinal lymph nodes in patients with lung squamous-cell carcinoma or adenocarcinoma.Lung Cancer. 2014 Apr 18.【原文下载】
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#PE#
26
#淋巴结#
35
#淋巴结转移#
42
#PET/CT#
42
#PET#
33
#评价#
29