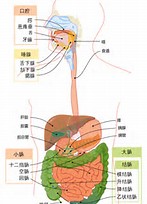
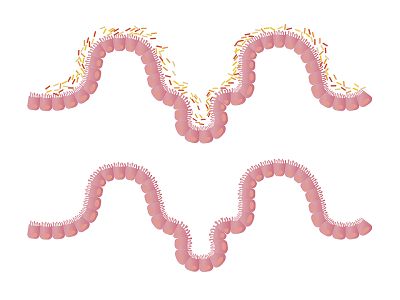
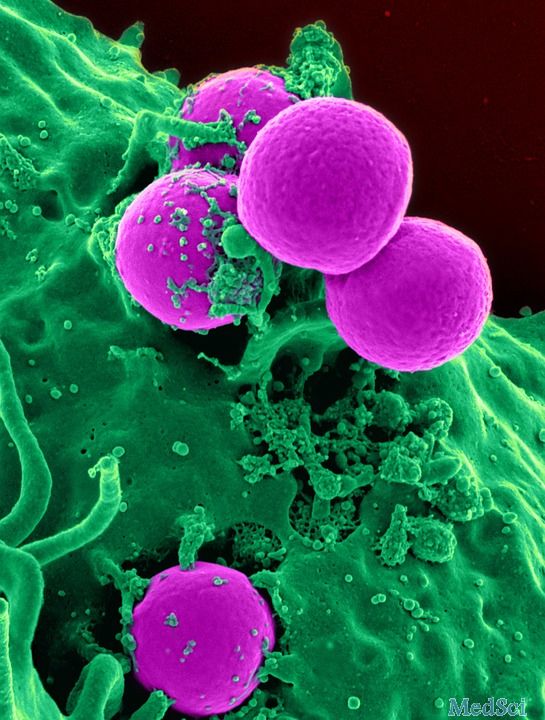
Am J Gastroenterol:肠炎患者肠道肿瘤风险因素研究
2017-05-29 zhangfan MedSci原创
研究认为,免疫抑制及抗TNF药物不会增加炎症性肠病患者肠道肿瘤风险,高龄及吸烟是该类患者肿瘤高风险因素
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#肿瘤风险#
28
#AST#
27
#Gastroenterol#
27
#肠道肿瘤#
34
#GAS#
24
到说的是肠外肿瘤还是肠道肿瘤?
64
认真学习,把间接经验应用到临床实践中去,然后再总结出新思路。给点赞啦
56
学习了,谢谢分享
63
学习了分享了
47
吸烟的危害!
47