PLoS One:中国汉族女性乳腺癌促炎症因子多态性关联分析
2012-04-10 Deepblue 生物谷
目前,乳腺癌病因学的研究主要集中在免疫及炎症方面。已知促炎症因子IL-17A和IL-17F能够介导炎症和癌症的发生。为了评估在乳腺癌风险中IL-17A和IL-17F基因多态性的作用,来自中国哈尔滨医科大学肿瘤预防及治疗中心的庞达教授及其课题组在中国汉族女性中开展了一个乳腺癌病例对照研究。研究发现,IL-17A中的单核苷酸多态性与乳腺癌发生风险有关。相关文章发表在3月26日的美国《公共科学图书馆·综

目前,乳腺癌病因学的研究主要集中在免疫及炎症方面。已知促炎症因子IL-17A和IL-17F能够介导炎症和癌症的发生。为了评估在乳腺癌风险中IL-17A和IL-17F基因多态性的作用,来自中国哈尔滨医科大学肿瘤预防及治疗中心的庞达教授及其课题组在中国汉族女性中开展了一个乳腺癌病例对照研究。研究发现,IL-17A中的单核苷酸多态性与乳腺癌发生风险有关。相关文章发表在3月26日的美国《公共科学图书馆·综合》(PLoS One)上。
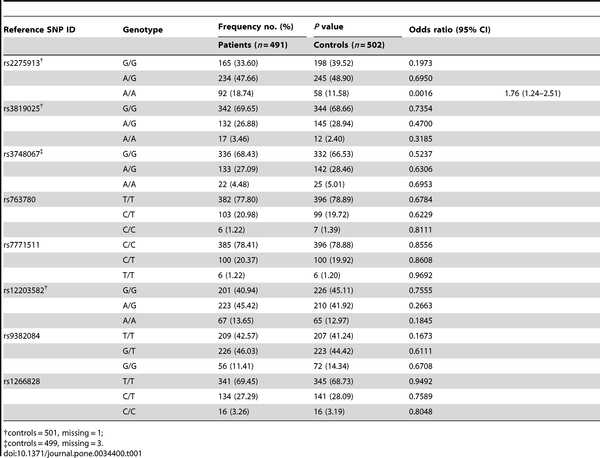
研究人员通过在IL-17A中发现的3个单核苷酸多态性(SNPs)(rs2275913, rs3819025 and rs3748067),以及在IL-17F中发现的5个SNPs(rs7771511, rs9382084, rs12203582, rs1266828和 rs763780),来确定在491个女性乳腺癌患者及502个健康个体中的单体型。通过SNaPshot技术研究者确定了基因型。而肺癌患者及健康个体的基因型分布差异则通过卡方检验被分析。
结果发现,对IL-17A中的rs2275913,AA基因型的频率高于控制组(P = 0.0016)。临床特征分析阐明了IL-17 SNPs与肿瘤蛋白53(P53)、黄体酮受体(PR)、人类表皮生长因子受体2 (Her-2)以及三阴状态(ER-/PR-/Her-2-)之间显著的联系。
除此之外,单体型分析表明了单体型Ars2275913Grs3819025Grs3748067的频率,位于IL-17A连锁不平衡模块,在患者中高于控制组(P = 0.0471)。
这项结果表明,IL-17A中的SNPs而不是IL-17F,与乳腺癌发生风险有关。总之,IL-17A及IL-17F的基因多态性可以提供有价值的信息,来推测中国女性乳腺癌的预后。(生物谷Deepblue编译)

doi: 10.1371/journal.pone.0034400
PMC:
PMID:
Association Analysis of IL-17A and IL-17F Polymorphisms in Chinese Han Women with Breast Cancer
Lihong Wang, Yongdong Jiang, Youxue Zhang, Yuwen Wang, Sunhui Huang, Zhihua Wang, Baoling Tian, Yue Yang, Wei Jiang, Da Pang.
Research into the etiology of breast cancer has recently focused on the role of the immunity and inflammation. The proinflammatory cytokines IL-17A and IL-17F can mediate inflammation and cancer. To evaluate the influences of IL-17A and IL-17F gene polymorphisms on the risk of sporadic breast cancer, a case-control study was conducted in Chinese Han women.We genotyped three single-nucleotide polymorphisms (SNPs) in IL-17A (rs2275913, rs3819025 and rs3748067) and five SNPs in IL-17F (rs7771511, rs9382084, rs12203582, rs1266828 and rs763780) to determine the haplotypes in 491 women with breast cancer and 502 healthy individuals.The genotypes were determined using the SNaPshot technique. The differences in the genotypic distribution between breast cancer patients and healthy controls were analyzed with the Chi-square test for trends.For rs2275913 in IL-17A, the frequency of the AA genotype was higher in patients than controls (P = 0.0016). The clinical features analysis demonstrated significant associations between IL-17 SNPs and tumor protein 53 (P53), progesterone receptor (PR), human epidermal growth factor receptor 2 (Her-2) and triple-negative (ER-/PR-/Her-2-) status.In addition, the haplotype analysis indicated that the frequency of the haplotype Ars2275913Grs3819025Grs3748067, located in the IL-17A linkage disequilibrium (LD) block, was higher in patients than in controls (P = 0.0471 after correction for multiple testing).Our results suggested that SNPs in IL-17A but not IL-17F were associated with the risk of breast cancer.Both IL-17A and IL-17F gene polymorphisms may provide valuable information for predicting the prognosis of breast cancer in Chinese women.<.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Plos one#
38
#促炎#
37
#促炎症因子#
40
#多态性#
32