ACC/AHA/HFSA 2022:推荐SGLT-2抑制剂用于治疗心衰
2022-04-03 Allan MedSci原创
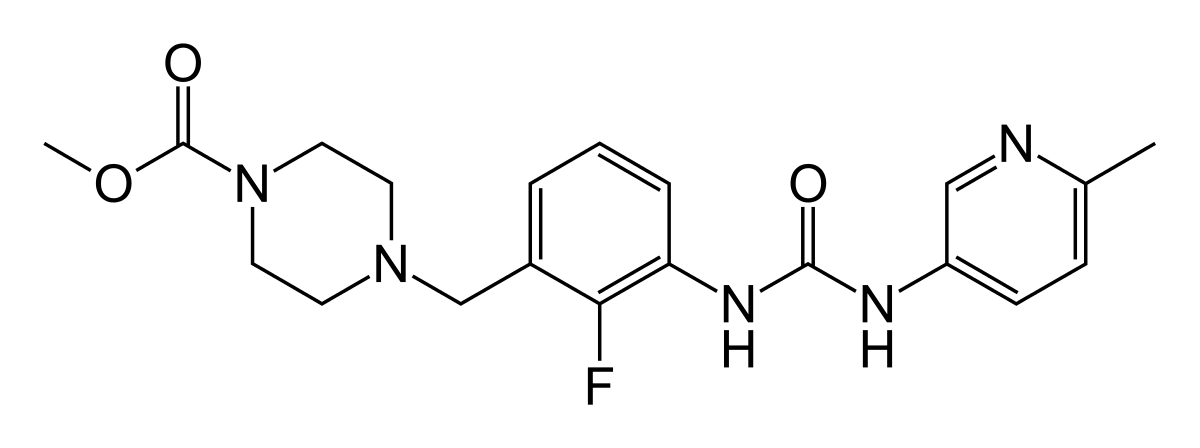
无论糖尿病状况如何,DAPA-HF 和 EMPEROR-HF 试验都证明用 SGLT-2 抑制剂治疗 HFrEF 患者的益处,显示心力衰竭再住院率降低了 30%。
心衰不是一种独立的心脏疾病,而是各种心脏疾病发展到严重阶段的一种临床综合征。它是由于各种病因导致的心脏功能减退,使心脏排血量减少,不能满足身体各组织器官需要而引起的一系列体征。
最新的联合指南由美国心脏病学会 (ACC)、美国心脏协会 (AHA) 和美国心力衰竭协会于上周五发布。更新后的美国指南推荐 SGLT-2 抑制剂治疗射血分数降低的症状性慢性心力衰竭 (HFrEF) 患者,无论他们是否患有 2 型糖尿病。
指南编写委员会副主席 Biykem Bozkurt 说:“在对新证据进行仔细评估后,指南指导的药物治疗现在包括四种药物类别,其中包括 SGLT-2 抑制剂、ACE 抑制剂、ARN 抑制剂和血管紧张素受体阻滞剂”。
Biykem Bozkurt 进一步指出:“无论糖尿病状况如何,DAPA-HF 和 EMPEROR-HF 试验都证明用 SGLT-2 抑制剂治疗 HFrEF 患者的益处,显示心力衰竭再住院率降低了 30%。SGLT-2 抑制剂在降低这一弱势群体的死亡率方面向前迈出了一大步”。
根据 DAPA-HF 试验的结果,FDA 于 2020 年批准了阿斯利康的 SGLT-2 抑制剂 Farxiga(达格列净),以降低 HFrEF 成人心血管(CV)死亡和心力衰竭住院的风险,且无论 2 型糖尿病状态如何。与此同时,今年早些时候,FDA 批准了另一种 SGLT-2 抑制剂 Jardiance(empagliflozin),以降低成人心血管死亡和心力衰竭住院的风险,且无论射血分数如何。Jardiance 的批准也得到了 III 期 EMPEROR-Reduced 和 EMPEROR-Preserved 研究数据的支持。
新指南发表在美国心脏病学会杂志上,也首次为射血分数在 41% 至 49% 之间的“轻度降低”患者以及射血分数保留 (HFpEF) 的患者提供治疗建议。根据最新的建议,两类患者都将受益于 SGLT-2 抑制剂。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#SGLT-2抑制#
41
#2抑制剂#
61
#SGLT-2#
50
#抑制剂#
38
#SGLT#
37
#AHA#
39
#ACC#
30