J Clin Pathol:病理评估——Cushing综合征分型的金标准
2014-11-30 MedSci译 MedSci原创
内源性Cushing综合征是一种罕见的内分泌紊乱疾病。由于糖皮质激素分泌过多,可以引起心血管疾病,甚至导致死亡。引起Cushing综合征的疾病分为肾上腺(20%)及非肾上腺(80%)源性。虽然大部分病例都是由于垂体病变或异位促肾上腺皮质激素(ACTH)过表达引起的,原发性肾上腺病变导致的皮质醇增多症在Cushing综合征病理生理学发病机制中越来越受到重视。最近十年我们对这一疾病的了解有了大幅度的提
内源性Cushing综合征是一种罕见的内分泌紊乱疾病。由于糖皮质激素分泌过多,可以引起心血管疾病,甚至导致死亡。引起Cushing综合征的疾病分为肾上腺(20%)及非肾上腺(80%)源性。虽然大部分病例都是由于垂体病变或异位促肾上腺皮质激素(ACTH)过表达引起的,原发性肾上腺病变导致的皮质醇增多症在Cushing综合征病理生理学发病机制中越来越受到重视。

图1 库兴氏综合征的临床特征
最近十年我们对这一疾病的了解有了大幅度的提升。最近,由于发现了环磷酸腺苷信号转导、ARMC5(一个假定的肿瘤抑制基因)、异常的G蛋白偶联受体和肾上腺内ACTH分泌等基因突变的情况,科学家们就肾上腺皮质醇增多症的发病机制提出了重要理论。
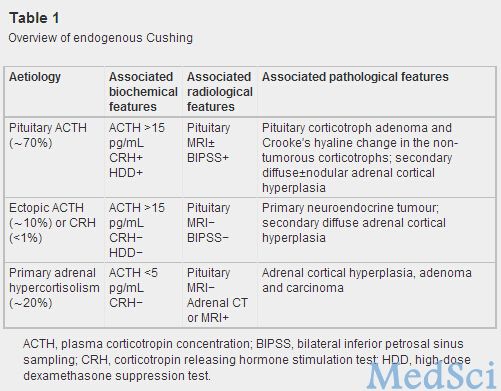
对Cushing综合征亚型的正确判断对制定治疗方案极为重要,这要求我们对临床、生化、影像学和病理结果进行整合。肾上腺的病理学相关因素包括肾上腺病理性增生、肾上腺腺瘤和肾上腺癌。虽然Cushing综合征最常见的表现为继发于ACTH产生过量的弥漫性肾上腺皮质增生,对这种疾病的治疗通常采用垂体或异位肿瘤切除术。面对Cushing综合征患者的肾上腺切除术后标本时,外科病理学家最常接触到的是肾上腺皮质腺瘤、肾上腺皮质癌和原发性大结节或小结节增生。
弥漫性增生
结节增生
肾上腺皮质腺瘤
肾上腺皮质癌
这篇文章对肾上腺Cushing综合征快速发展的相关知识进行了更新,并对这一重要疾病的临床病理联系进行了讨论。结合临床、生化和影像学的研究结果进行综合考虑,彻底的病理评估将成为对Cushing综合征进行分型和管理的金标准。
原始出处:
Duan K1, Gomez Hernandez K2, Mete O3.Clinicopathological correlates of adrenal Cushing's syndrome.J Clin Pathol. 2014 Nov 25. pii: jclinpath-2014-202612. doi: 10.1136/jclinpath-2014-202612. [Epub ahead of print]
本文为MedSci原创编译,欢迎转载,转载请注明出处并附上原文链接
您还可以这样阅读,更多资讯,请关注MedSci微信


版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Pathol#
22
好好学习学习
113
#金标准#
29
#病理评估#
34
#综合征#
31