JAHA:减少血管损伤后内膜新生的新靶点!
2017-06-27 MedSci MedSci原创
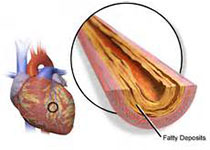
尽管血管成形术和药物洗脱支架在治疗动脉粥样硬化中的效果最近有所改善,但再狭窄和支架内血栓形成仍是常见的并发症并导致许多死亡。因此,阻断再狭窄的新分子靶点的研究显得尤为重要。近日,在国际心血管权威杂志JAHA上发表了一篇旨在建立血管生成因子AGGF1(血管生成因子)作为阻断新生内膜形成和血管损伤再狭窄的新靶点。
尽管血管成形术和药物洗脱支架在治疗动脉粥样硬化中的效果最近有所改善,但再狭窄和支架内血栓形成仍是常见的并发症并导致许多死亡。因此,阻断再狭窄的新分子靶点的研究显得尤为重要。近日,在国际心血管权威杂志JAHA上发表了一篇旨在建立血管生成因子AGGF1(血管生成因子)作为阻断新生内膜形成和血管损伤再狭窄的新靶点。
AGGF1在颈动脉中表达较高,但是其血管损伤后的动脉的表达明显下降。 AGGF1 +/-小鼠显示增加的新生内膜形成伴随着血管损伤后颈动脉血管平滑肌细胞(VSMC)的增加。另外,AGGF1的蛋白治疗可以通过抑制增殖并促进VSMCs在小鼠体内收缩表型的表型转换来阻断血管损伤后的新内膜形成。在体外,AGGF1显着抑制VSMC的增殖,并降低S期的细胞数。 AGGF1还阻断血小板衍生生长因子-BB诱导的增殖、VSMC的迁移、增加细胞周期蛋白D的表达,并降低p21和p27的表达。 AGGF1通过抵抗血小板衍生生长因子-BB对SRF表达的抑制作用以及参与VSMCs标志物活化的心肌素/SRF/CArG盒复合物的形成,抑制VSMCs对合成表型的表型转换。最后,本研究显示AGGF1抑制血小板衍生生长因子-BB诱导的MEK1/2,ERK1/2的磷酸化和参与VSMC表型转换的Elk磷酸化,并且Elk的过度表达消除了AGGF1的作用。
通过调节新型的AGGF1-MEK1/2-ERK1/2-Elk-心肌素-SRF/
p27信号通路,AGGF1蛋白治疗可有效阻断血管损伤后的新内膜形成。
原始出处:
Yu Y et al.Targeting AGGF1 (angiogenic factor with G patch and FHA domains 1) for Blocking Neointimal Formation After Vascular Injury.JAHA.2017 June.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#内膜#
21
#血管损伤#
25
#AHA#
27
#新靶点#
29
#损伤#
26
非常好的文章,学习了,很受益
46
签到学习了很多。
65
通过调节新型的AGGF1-MEK1/2-ERK1/2-Elk-心肌素-SRF/p27信号通路,AGGF1蛋白治疗可有效阻断血管损伤后的新内膜形成。
53