PLoS Biology:研究发现转录因子可导致乳腺癌对抗雌激素治疗无应答
2013-01-07 PLoS Biology dxy zhihui_li
澳大利亚的科学家们已经证实一种“转录因子”如何引起乳腺癌进展为侵袭性亚型,而且这种亚型缺乏对雌激素的敏感性,同时对于像他莫昔芬和芳香酶抑制剂这样的抗雌激素药物治疗无效。 转录因子是一类可以转换基因的“开”或“关”的分子。在这种情况下,所熟知的转录因子“ELF5”在乳腺癌细胞的极早期抑制其对雌激素的敏感性。2008年,来自悉尼Garvan医学研究所的副教授Chris Orma
澳大利亚的科学家们已经证实一种“转录因子”如何引起乳腺癌进展为侵袭性亚型,而且这种亚型缺乏对雌激素的敏感性,同时对于像他莫昔芬和芳香酶抑制剂这样的抗雌激素药物治疗无效。
转录因子是一类可以转换基因的“开”或“关”的分子。在这种情况下,所熟知的转录因子“ELF5”在乳腺癌细胞的极早期抑制其对雌激素的敏感性。2008年,来自悉尼Garvan医学研究所的副教授Chris Ormandy证实ELF5负责刺激生成乳腺内雌激素受体阴性的细胞,可以在妊娠期间产生乳汁。
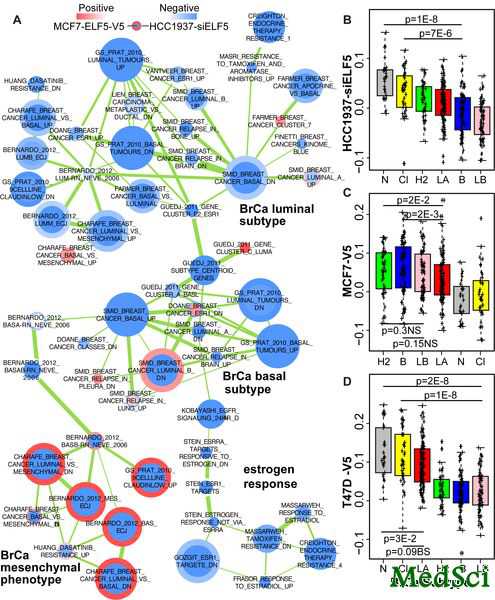
Ormandy在当前的研究中,与Maria Kalyga博士和David Gallego-Ortega博士一道证实,同样的分子决定了乳腺癌的发生,并且ELF5可以将现发生的肿瘤改变为雌激素不敏感型。研究小组已经描述了ELF5通过怎样的遗传机制来对抗雌激素的作用,同时也证实通过操纵ELF5水平来改变乳腺癌亚型是有可能的。研究结果现已在线发表于具有很大影响力的杂志—PLoS Biology上。
Ormandy说:“这项工作告诉我们,癌症之所以会变成抗雌激素难治性,就是因为它们经常借助抬高ELF5水平,从而变为功能性的雌激素受体阴性。这就引出了一个新的治疗选择,即通过操纵ELF5水平来治疗乳腺癌。由于ELF5是胞内的,使用可以靶向产生蛋白质-蛋白质相互作用的小分子或许可以达到目的,或者使用小的抑制性RNAs。同时,通过检测肿瘤内ELF5的含量水平来预测对治疗的反应,并因此指导治疗选择也是可能的。这里我们关键的发现就是借助简单地操纵一种转录因子,我们可以改变乳腺癌的亚型。”
ELF5 Suppresses Estrogen Sensitivity and Underpins the Acquisition of Antiestrogen Resistance in Luminal Breast Cancer
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Bio#
36
#研究发现#
36
#Biol#
29
#无应答#
29
#转录#
37
#雌激素治疗#
0
#激素治疗#
50
#转录因子#
31