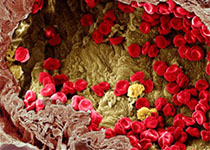
ASCO: 让我们等待已久、感动得要哭的肿瘤新药!
2017-06-05 蚂蚁 Haalthy肺腾助手
ASCO大会1LOXO-101: 实体瘤和儿童肿瘤的TRK抑制剂55名有TRK融合的肿瘤病人(年龄从4个月到76岁,是的,其中包括4个月的宝宝)参与了这个临床试验,其中唾液腺癌12人,肉瘤10人,先天性婴儿纤维肉瘤7人,肺癌5人,甲状腺瘤5人,大肠癌4人,黑色素瘤4人,胆管癌2人,胃肠道基质瘤2人和其他肿瘤4人。在46名能够评估的患者中,客观有效率(ORR)为78%,完全缓解(CR)12%。另外,

55名有TRK融合的肿瘤病人(年龄从4个月到76岁,是的,其中包括4个月的宝宝)参与了这个临床试验,其中唾液腺癌12人,肉瘤10人,先天性婴儿纤维肉瘤7人,肺癌5人,甲状腺瘤5人,大肠癌4人,黑色素瘤4人,胆管癌2人,胃肠道基质瘤2人和其他肿瘤4人。在46名能够评估的患者中,客观有效率(ORR)为78%,完全缓解(CR)12%。另外,有88%的肿瘤仍然有应答,最长的应答时间为23个月!
2 ALRN-6924: 实体瘤的MDM2/MDMX抑制剂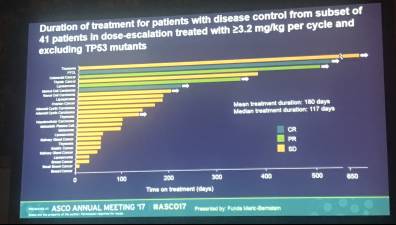
41名可评估的无TP53突变的实体瘤病人中,疾病控制率为59%,其中有两名患者完全缓解。最关键的是,这些药物的中位治疗期达到了180天,其中有患者已经持续用药2年多。
3 CH5126766:非小细胞肺癌的KRAS突变抑制剂肺癌中的Kras突变一直是最难搞的突变之一:没有靶向药,也没有十分有效的化疗药。
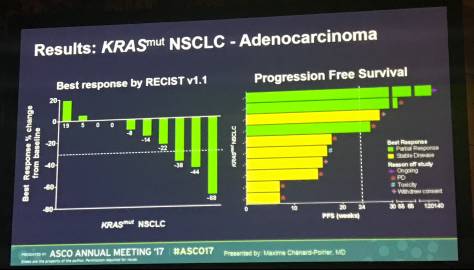
这个由罗氏研发的针对Kras突变的新药CH5126766,在2017ASCO上公布的数据显示,效果较为让人满意,而且安全性较高。其中一名对CH5126766有效的肺癌病人,肿瘤缩小达68%!!令人更加惊喜的是,最长的无疾病进展期(PFS)达140周,即2年有余!而且到数据截止日起,患者依然对药物有应答。
4 Ulixertinib: 实体瘤的ERK1/2抑制剂Ulixertinib是针对MAPK通路(ERK1/2信号通路)的新型靶向药,此通路可能有BRAFV600和RAS突变的存在。在I期的临床中,包含了101名直肠癌、非小细胞肺癌、黑色素瘤和其他有BRAF突变的肿瘤。
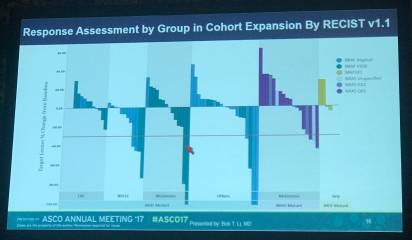
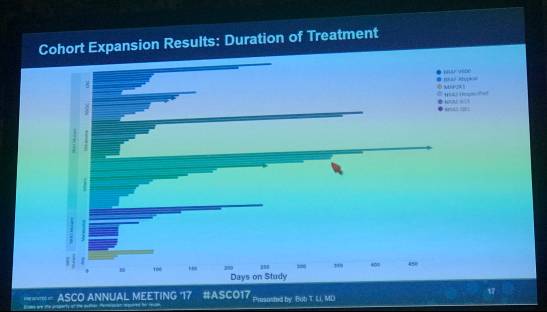
其中,有14%的患者有应答,在BRAF突变的非小细胞肺癌和黑色素瘤中的应答较佳,最长应答时间超过3年!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#肿瘤新药#
38
#ASC#
25
学习了,点赞
73
针对Kras突变的新药CH5126766,关注在肠癌中的表现
75
学习了,谢谢分享
84
共同学习共同进步!
67
讲的非常好,非常期待,期待中
68
优质资源,共同学习共同进步
29