Hepertension:Nrf2基因缺失对高血压的影响
2017-05-06 MedSci MedSci原创
核因子红细胞2相关因子2(Nrf2)是氧化还原稳态的主转录调节因子,它可以影响抗氧化基因的表达。延髓头端腹外侧(RVLM)的中枢氧化应激和抗氧化酶的表达降低促进慢性心力衰竭中的交感神经激活。近期,一项发表在杂志Hypertension上的研究评估了RVLM中Nrf2的缺失是否增加交感神经驱动力和血压。研究者们将慢病毒-Gre-GFP或慢病毒-GFP微量注射至Nrf2- floxed小鼠中的RVLM
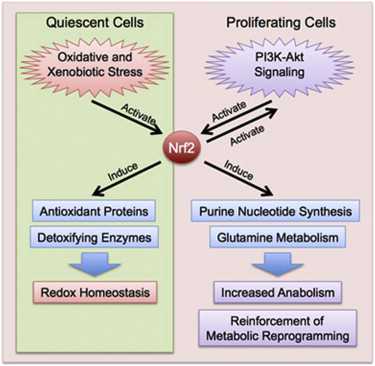
核因子红细胞2相关因子2(Nrf2)是氧化还原稳态的主转录调节因子,它可以影响抗氧化基因的表达。延髓头端腹外侧(RVLM)的中枢氧化应激和抗氧化酶的表达降低促进慢性心力衰竭中的交感神经激活。
近期,一项发表在杂志Hypertension上的研究评估了RVLM中Nrf2的缺失是否增加交感神经驱动力和血压。
研究者们将慢病毒-Gre-GFP或慢病毒-GFP微量注射至Nrf2- floxed小鼠中的RVLM。2周后,评估Nrf2信号、蛋白质、氧化应激、心血管功能和交感神经。
研究者们发现,与对照组的GFP小鼠相比,(1)RVLM中的Nrf2 mRNA和蛋白质在Cre小鼠中显着较低。Nrf2靶向的抗氧化酶下调,而活性氧提高。(2)血压测量结果表明,Cre小鼠血压显着升高(平均动脉压为123.7±3.8 vs. 100.2±2.2 mm Hg; P <0.05,n = 6),尿中去甲肾上腺素(NE)浓度升高(456.4 ±16.9 vs. 356.5±19.9ng / mL; P <0.05,n = 6),自发压力反射增益降低(上升序列为1.66±0.17 vs. 3.61±0.22ms / mm Hg; P <0.05,n = 6; 下降序列为1.89±0.12 vs. 2.98±0.19 ms / mm Hg; P <0.05,n = 6)。(3)Cre小鼠显示出升高的基线肾交感神经活动和受损的诱导型压力反射功能。
此项研究数据表明RVLM中的Nrf2基因缺失可以升高血压,增加交感神经流出,并且通过受损的抗氧化酶表达潜在地损害了压力反射功能。
原始出处:
Gao L, Zimmerman MC, et al. Selective Nrf2 Gene Deletion in the Rostral Ventrolateral Medulla Evokes Hypertension and Sympathoexcitation in Mice. Hypertension. 2017 May 1. pii: HYPERTENSIONAHA.117.09123. doi: 10.1161/HYPERTENSIONAHA.117.09123.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#PE#
32
#基因缺失#
42
#TENS#
36
#Nrf2#
53
认真学习,把间接经验应用到临床实践中去,然后再总结出新思路。点赞啦!
75
好的,不错
92
感谢分享一下!!
85
学习一下谢谢分享
81