专家呼吁建立精准医学发展共享机制
2016-06-21 李晨阳 中国科学报
6月16日~17日,以“精准医学与肿瘤治疗”为主题的首届雁栖湖医学高峰论坛在京召开。会上,中国工程院院士、北大医学部主任詹启敏指出,发展精准医学需要建立医院间的共享机制,破除各单位“各立门派”、互不往来的弊端。 詹启敏介绍说,精准医学的一大重要支撑平台是“大数据平台”。通过聚集海量的队列数据、临床数据、组学数据、结构生物学数据、药物分子信息,再经由生物信息技术处理,才能发现新靶点、新结构,
6月16日~17日,以“精准医学与肿瘤治疗”为主题的首届雁栖湖医学高峰论坛在京召开。会上,中国工程院院士、北大医学部主任詹启敏指出,发展精准医学需要建立医院间的共享机制,破除各单位“各立门派”、互不往来的弊端。
詹启敏介绍说,精准医学的一大重要支撑平台是“大数据平台”。通过聚集海量的队列数据、临床数据、组学数据、结构生物学数据、药物分子信息,再经由生物信息技术处理,才能发现新靶点、新结构,设计新药物、新方案,进而推进新标准和新规范的制定。
然而,信息孤岛现象阻碍了上述进程。北京大学肿瘤医院院长季加孚指出,精准医学的肿瘤研究平台需要成规模、高水平的集团协同。这种协同的前提是具备普遍约束力的规范、便于共享的环境和可靠的质量监管。相应地,现有的激励、管理制度也应随之调整。
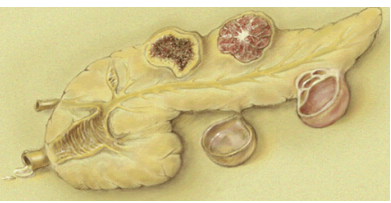
建立和共享生物样本库,也是此次论坛热议的话题之一。詹启敏表示,生物样本不仅需要符合严格的质量要求,还必须匹配完整、真实、标准化的临床信息。然而,由于种种原因,目前我国临床信息资料的质量不容乐观,是必须迫切解决的问题之一。
此次论坛由中国科学院大学和北京市怀柔区政府主办,国科大医学院和国科大附属北京怀柔医院承办。众多两院院士及国内外专家学者参会并作学术报告。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#专家呼吁#
42
#医学发展#
47
非常好。
128
#精准#
37
#共享#
52