Nat Commun:血管紧张素Ⅱ或可预测H7N9致命程度
2014-05-13 朱涵、张乐 新华网
科学家的一项最新研究发现,存在人体血浆中的一种蛋白“血管紧张素Ⅱ”和H7N9禽流感的病死率相关,“血管紧张素Ⅱ”指标越高,H7N9禽流感患者病死率越高。 这项研究成果由浙江大学医学院附属第一医院联合中国医学科学院、中国疾病预防控制中心的科研人员共同完成,于北京时间5月6日23时发表于《自然·通讯》杂志。这也是科学家首次发现并报道单个蛋白与H7N9禽流感疾病之间的相关性。 “血管紧张素Ⅱ”存在于
科学家的一项最新研究发现,存在人体血浆中的一种蛋白“血管紧张素Ⅱ”和H7N9禽流感的病死率相关,“血管紧张素Ⅱ”指标越高,H7N9禽流感患者病死率越高。
这项研究成果由浙江大学医学院附属第一医院联合中国医学科学院、中国疾病预防控制中心的科研人员共同完成,于北京时间5月6日23时发表于《自然·通讯》杂志。这也是科学家首次发现并报道单个蛋白与H7N9禽流感疾病之间的相关性。
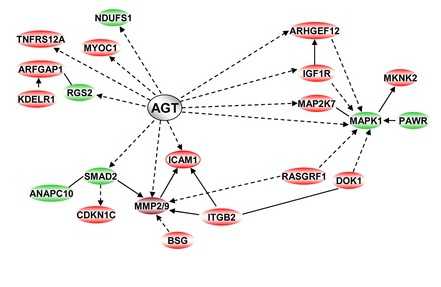
“血管紧张素Ⅱ”存在于人体血浆、血管壁、心脏、肾脏等组织中,主要功能是调节机体血压、维持水电解质平衡,同时与急性肺损伤的发生、发展关系密切。
研究团队收集了杭州、上海、南京三地的47例H7N9禽流感确诊患者的血浆,研究人员发现,H7N9禽流感病重患者血浆中的“血管紧张素Ⅱ”显著高于对照组,且“血管紧张素Ⅱ”水平越高,体内的病毒载量越多。
“这一特征在发病后第二周尤为明显。包括8例死亡患者在内的重症患者‘血管紧张素Ⅱ’指标普遍保持上升状态,但轻症患者的这一指标在第二周就会有所下降。”该成果的领衔者、国家卫生和计生委人感染H7N9禽流感疫情防控工作专家组专家李兰娟表示。
此外,进一步研究发现,与此前检测的C反应蛋白、氧合指数等临床指标相比,“血管紧张素Ⅱ”预测H7N9禽流感严重程度与是否致命的准确度更高。
在此之前,由于缺乏足够大样本的分析统计,研究人员很难发现单个蛋白在人血浆中的改变与疾病严重程度及发展情况的关系,临床上也没有预测H7N9禽流感病毒感染疾病的严重程度以及疾病进展情况的标志物。
“此次发现可令这种蛋白用于临床,作为首个H7N9患者重症化的预警指标,预测患者疾病的致命程度。”李兰娟说,这将有助于医护人员根据病情不同的患者采取不同的抢救措施,从而令治疗更加可靠、有效。
2013年3月,中国在全球首先报告发现H7N9禽流感病毒,该病毒可由禽传染给人,引发重症肺炎并危及生命。从2013年3月至今,中国各地报告的禽流感病例已经超过200例。
李兰娟研究团队2013年介入H7N9禽流感研究以来,进行了一系列研究,发现活禽市场是人类感染H7N9的主要源头,发现导致H7N9禽流感由禽传人的病毒基因变异位点,首次揭示了H7N9感染临床规律性特征、患者的病例特征,并成功自主研发H7N9禽流感病毒疫苗株,开发了快速诊断试剂盒。
原始出处
Huang F1, Guo J2, Zou Z1, Liu J3, Cao B4, Zhang S5, Li H6, Wang W7, Sheng M7, Liu S7, Pan J8, Bao C9, Zeng M10, Xiao H11, Qian G12, Hu X12, Chen Y12, Chen Y12, Zhao Y7, Liu Q7, Zhou H7, Zhu J7, Gao H12, Yang S12, Liu X12, Zheng S12, Yang J12, Diao H12, Cao H12, Wu Y13, Zhao M13, Tan S13, Guo D14, Zhao X15, Ye Y15, Wu W15, Xu Y14, Penninger JM16, Li D17, Gao GF18, Jiang C19, Li L12.Angiotensin II plasma levels are linked to disease severity and predict fatal outcomes in H7N9-infected patients.Nat Commun. 2014 May 6;
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#COMMUN#
37
#Nat#
33
#H7N9#
26
#血管紧张素#
43