Diabetes Care:糖尿病合并COPD患者应谨慎使用皮质激素类药物
2013-06-17 Diabetes Care dxy
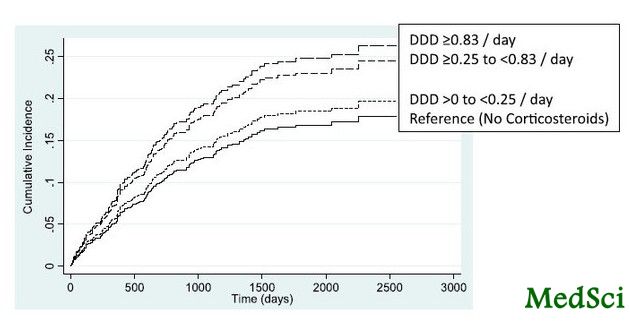
经不同剂量皮质激素分层,因糖尿病并发症住院累积发生率 为了确定采用皮质激素治疗的糖尿病合并慢性阻塞性肺病(COPD)患者糖尿病并发症风险是否呈剂量依赖性增加。来自南澳大利亚大学药学和医学科学院药品使用质量和药学研究中心的Gillian E. Caughey博士等人进行了一项研究,研究发现,糖尿病合并COPD患者使用高剂量皮质激素时糖尿病相关住院风险明显增高。研究结果在线发表于2013年6月4日美
为了确定采用皮质激素治疗的糖尿病合并慢性阻塞性肺病(COPD)患者糖尿病并发症风险是否呈剂量依赖性增加。来自南澳大利亚大学药学和医学科学院药品使用质量和药学研究中心的Gillian E. Caughey博士等人进行了一项研究,研究发现,糖尿病合并COPD患者使用高剂量皮质激素时糖尿病相关住院风险明显增高。研究结果在线发表于2013年6月4日美国的《糖尿病治疗》(Diabetes Care)杂志上。
这是一项对2001年7月至2008年6月澳大利亚政府退伍军人事务部康管理索赔数据库中记录人群进行的回顾性研究,研究中的糖尿病患者刚开始使用二甲双胍或磺酰脲类药物。COPD定义为研究开始前6个月使用噻托溴铵或异丙托溴铵。确定研究开始后12个月内皮质激素使用总量(吸入和全身给药)。研究结局为由于糖尿病并发症的入院时间。校正多个变量后,采用竞争风险和Cox比例风险回归分析法对结果进行评价。
结果显示,研究总共鉴定了18,226糖尿病患者,其中5.9%的患者有COPD。在这些COPD患者中,67.2%的患者自进入研究12个月内给予皮质激素治疗。与那些没有接受皮质激素的患者比较,不同剂量皮质激素分层显示,服用皮质激素总限定日剂量(DDD)≥0.83 /天的患者因糖尿病并发症住院的可能性增加94%(亚风险比1.94[95% CI 1.14-3.28],P=0.014)。低剂量皮质激素(<0.83DDD/天)与糖尿病相关住院风险增高没有关系。
研究发现,在糖尿病合并COPD患者中,糖尿病相关住院风险仅在使用高剂量皮质激素时明显增高。这突出了在治疗糖尿病合并COPD患者时,需要不断改变皮质激素用量,以确保使用最低有效剂量,同时应观察适当的治疗反应。

Comorbid Diabetes and COPD: Impact of corticosteroid use on diabetes complications.
OBJECTIVE
To identify if there is a dose-dependent risk of diabetes complications in patients treated with corticosteroids that have both diabetes and chronic obstructive pulmonary disorder (COPD).
RESEARCH DESIGN AND METHODSA
retrospective study of administrative claims data from the Australian Government Department of Veterans' Affairs, from 1 July 2001 to 30 June 2008, of diabetes patients newly initiated on metformin or sulfonylurea. COPD was identified by dispensings of tiotropium or ipratropium in the 6 months preceding study entry. Total corticosteroid use (inhaled and systemic) in the 12 months after study entry was determined. The outcome was time to hospitalization for a diabetes-related complication. Competing risks and Cox proportional hazard regression analyses were conducted with adjustment for a number of covariates.
RESULTS
A total of 18,226 subjects with diabetes were identified, of which 5.9% had COPD. Of those with COPD, 67.2% were dispensed corticosteroids in the 12 months from study entry. Stratification by dose of corticosteroids demonstrated a 94% increased likelihood of hospitalization for a diabetes complication for those who received a total defined daily dose (DDD) of corticosteroids ≥0.83/day (subhazard ratio 1.94 [95% CI 1.14-3.28], P = 0.014), by comparison with those who did not receive a corticosteroid. Lower doses of corticosteroid (<0.83 DDD/day) were not associated with an increased risk of diabetes-related hospitalization.
CONCLUSIONS
In patients with diabetes and COPD, an increased risk of diabetes-related hospitalizations was only evident with use of high doses of corticosteroids. This highlights the need for constant revision of corticosteroid dose in those with diabetes and COPD, to ensure that the minimally effective dose is used, together with review of appropriate response to therapy.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Diabetes#
27
#BET#
34
#DIA#
30
#COPD患者#
27
#皮质激素#
29