


本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
2018-04-09 韩博 李尚慧 赵国栋 北京口腔医学
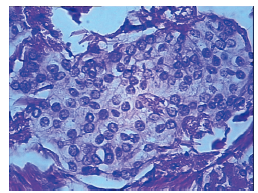
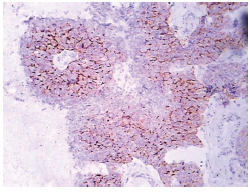
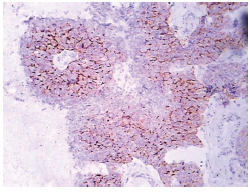
患者,女,65岁,2013-10-29因右腋下肿物2个月入院。




2018年3月21日,第11届欧洲乳腺癌大会(EBCC-11)于西班牙巴塞罗那举行。会议第二天上午,来自荷兰、意大利等国家的讲者分别对乳腺癌寡转移病灶的生物学特性、局部治疗价值、颅内外寡转移灶的局部处理方式进行了系统梳理,现将报告精要整理如下。
近日,《细胞》杂志子刊《分子细胞》(Molecular Cell)在线发表了厦门大学药学院刘文教授课题组的研究成果“JMJD6 Licenses Estrogen Receptor α-Dependent Enhancer and Coding Gene Activation by Modulating the Recruitment of the CARM1/MED12 Co-activator
近日,Nature旗下的肿瘤学领域著名国际期刊Oncogene在线发表了厦门大学药学院王团老教授课题组的研究性论文“Rab34 regulates adhesion, migration, and invasion of breast cancer cells”。该成果首次揭示了小分子GTP酶Rab34参与调控乳腺癌的相关功能和机制。
大约在100年前,著名的生理学家Otto Warburg教授与他的同事们发现了癌细胞一个有趣的现象:和正常细胞相比,癌细胞要消耗更多的葡萄糖。这听起来很合理——癌细胞是一类需要快速分裂和增殖的恶性细胞,当然需要更多的能量。
肿瘤微环境(TME)可以促进肿瘤细胞的侵袭和转移。促癌微环境转化的一个重要步骤是正常基质成纤维细胞向癌相关成纤维细胞(CAF)的转化。
20 世纪80 年代,蒽环类药物(anthracyclines)以其卓越的疗效成为乳腺癌术后辅助化疗的里程碑。在新型药物涌现、多种治疗模式并存的循证医学时代,即使重新审视,仍可发现蒽环类药物不仅在乳腺癌术后辅助化疗中占有极其重要的地位,而且在新辅助化疗、晚期乳腺癌患者治疗中也据有一席之地。为了进一步明确蒽环类药物在乳腺癌中的治疗作用,准确评估蒽环类药物的临床疗效及不良反应,减少治疗的盲目性并增强规


梅斯医学MedSci APP
医路相伴,成就大医
学习
75
学习了.谢谢作者分享!
71
#腮腺#
37
#口腔医学#
33
学习
65