Hypertension:收缩压与降压药依从性生化评估相关性分析!
2017-06-27 xing.T MedSci原创
抗高血压药物的生化评估可以帮助从其他升高血压的原因中区分出药物的依从性较差引起的血压升高,并确定需要进行干预的目标人群。
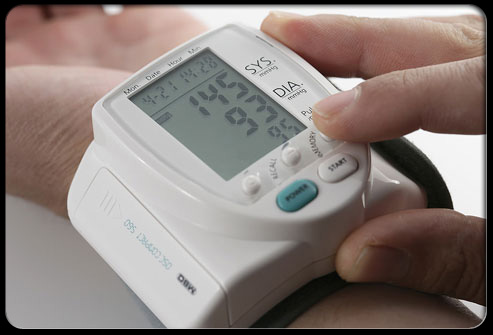
高血压在急诊科很是常见,但抗高血压药物的依从性与血压之间的关系尚不明确。近日,心血管权威杂志Hypertension上发表了一篇研究文章,这项横断面研究通过分析2012年7月至2013年4月期间在教学医院寻求高血压治疗的成年高血压患者,旨在检测了高血压患者较高的抗高血压药物的依从性与较低收缩压之间存在相关性的假设。
研究人员采用质谱法进行抗高血压药物依从性的生化评估,并且该研究的主要结局为急诊平均收缩压。调整年龄、性别、种族、保险、教育程度、算术、体重指数和合并症后,根据处方中抗高血压药物的数量(<3个,≥3个)进行分层分析。
在85例处方中≥3个抗高血压药的患者中,对于依从性较好的患者平均收缩压为134.4mmHg(±26.1mmHg),并在调整后的分析中,与依从性差的患者相差-20.8 mmHg(95%可信区间为34.2-7.4mmHg;P=0.003)。在176例处方中<3个抗高血压药物的患者,依从性较好的患者平均收缩压为135.5mmHg(±20.6mmHg),在调整分析中,依从性并未引起差异(+2.9mmHg;95%可信区间为-4.7-10.5mmHg;P=0.45)。生化评估确定的抗高血压药物不依从性较为常见,并且与有初级保健和健康保险并且处方中≥3个降压药物的患者较高的急诊收缩压相关。
抗高血压药物的生化评估可以帮助从其他升高血压的原因中区分出药物的依从性较差引起的血压升高,并确定需要进行干预的目标人群。
原始出处:
Candace D. McNaughton,et al. Systolic Blood Pressure and Biochemical Assessment of Adherence.Hypertension.2017. https://doi.org/10.1161/HYPERTENSIONAHA.117.09659
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#PE#
24
#相关性#
25
#收缩压#
37
#降压#
34
#依从性#
33
#Hypertension#
25
#相关性分析#
25
#TENS#
21
学习了分享了
64
合理规范的服用降压药
66