Immunity:重磅!视黄酸抑制结直肠癌产生
2016-08-31 佚名 生物谷
在一项新的研究中,来自美国斯坦福大学医学院的研究人员发现作为体内由维生素A产生的一种化合物,视黄酸在抑制小鼠和人类患上结直肠癌中发挥着至关重要的作用。相关研究结果于2016年8月30日在线发表在Immunity期刊上,论文标题为“Normalizing Microbiota-Induced Retinoic Acid Deficiency Stimulates Protective CD8+

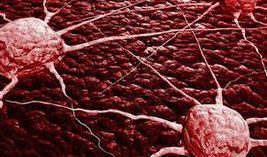
研究人员发现患有这种癌症的小鼠在它们的肠道中含有低于正常水平的视黄酸。再者,肠道组织表达高水平的降解视黄酸的蛋白的结直肠癌病人往往要比他们的同行表现得更差。
这项研究是首次揭示出视黄酸水平、免疫相关炎症和肠道微生物之间存在复杂的相互作用。它可能提示着新的方法来阻止或治疗结直肠癌病人。
论文通信作者、斯坦福大学医学院病理学与医学教授Edgar Engleman博士说,“肠道持续地遭受外来有机体的攻击。因此,它的免疫系统是非常复杂的。在人体内,包括溃疡性结肠炎在内的炎症性肠病与最终的结直肠癌产生之间存在明显的关联性。多年来,已知视黄酸参与抑制肠道中的炎症。我们想要将这些点连接在一起,了解视黄酸水平是否和如何直接地影响癌症产生。”
小鼠体内的肿瘤
视黄酸是很多生长和发育过程所必需的,但是当遭受光线照射时,它也很快地降解。这使得很难准确地检测体内的视黄酸水平。
在这项研究中,斯坦福大学研究人员与来自美国加州大学伯克利分校的同事们合作开展研究,其中后者开发出一种利用定量质谱技术测量经过两种化学物---一种化学物导致肠道炎症,一种化学物促进结直肠癌产生---中的一种或两种物质处理的小鼠肠道组织中的视黄酸水平。接受这两种化学物处理的小鼠在9到10周内患上肠道肿瘤;仅接受第一种化学物处理的小鼠产生肠道炎症,但是没有产生癌症。
Engleman和他的同事们发现患有结直肠癌的小鼠要比肠道产生炎症但未发生癌变的那些小鼠具有显著低于正常水平的视黄酸。进一步的研究表明患有结直肠癌的小鼠的肠道组织制造更少的一种合成视黄酸的蛋白,但会制造大约4倍多的一种降解视黄酸的蛋白,从而导致视黄酸水平快速地净下降。
恢复视黄酸水平
研究人员随后测试了通过让肠道组织中的视黄酸水平恢复到一种更加正常的范围是否可能影响这种疾病进展。
Engleman说,“当我们通过给这些小鼠添加视黄酸或者通过阻断这种降解酶的活性来增加肠道中的视黄酸水平时,我们能够显著地降低它们体内的肿瘤负荷。相反地,抑制视黄酸活性会显著地增加肿瘤负荷。”
研究人员接下来研究了储存的从患有溃疡性结肠炎或与溃疡性结肠炎相关联的结直肠癌的病人体内获得的肠道组织样品中的这种合成蛋白和这种降解蛋白的水平。鉴于这些样品已经过储存而不是新鲜收集的,因此直接测量这些人肠道组织样品中的视黄酸水平是不可能的。
研究人员发现类似于他们在小鼠体内观察到的情形,人结直肠癌组织要比仅仅产生炎症的人肠道组织具有更高水平的这种降解蛋白和更低水平的这种合成蛋白。再者,他们观察到这种降解蛋白的水平与病人的存活时间之间存在负相关性。换言之,肠道组织中这种降解酶水平增加的那些病人往往要比具有更少这种酶的其他人表现得更差。
鉴于研究人员也在来自患有结直肠癌但之前没有溃疡性结肠炎病史的病人的肠道组织样品中观察到类似的蛋白水平变化,他们想要知道是否可能存在另一种影响视黄酸水平的肠道炎症的病因。他们已知道肠道中天然存在的细菌有时能够导致局部炎症,并且猜测它们可能促进视黄酸缺乏和结直肠癌产生。利用广谱抗生素治疗这些小鼠来剔除这些细菌,会显著地降低几种结直肠癌模式小鼠体内的肿瘤形成,阻止在患有结直肠癌的小鼠和人结肠组织中观察到的视黄酸代谢变化。
Engleman说,“我们发现细菌,或者由细菌产生的分子,能够导致肠道中产生大规模的炎性反应,从而直接影响视黄酸代谢。在正常条件下,视黄酸水平受到非常紧密地调节。这一发现可能能够对治疗人结直肠癌产生重要影响。”
进一步研究证实视黄酸通过激活一类被称作CD8 T细胞的免疫细胞来阻断或延缓癌症产生。这些T细胞然后杀死这些癌细胞。研究人员发现,在小鼠体内,更低水平的视黄酸导致肠道组织中CD8 T细胞的数量和激活下降,而且增加这些小鼠体内的肿瘤负荷。
Engleman说,“通过之前开展过的很多研究,已经非常清楚的是,慢性炎症是很多癌症类型的一种非常重要的风险因子。鉴于我们已证实视黄酸缺乏在结直肠癌中所起的作用,我们想要鉴定出在人体中启动这些变化的特定微生物。最终,我们希望确定我们的发现是否可能能够被用来预防或治疗结直肠癌。”
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Immunity#
28
#酸抑制#
37
很好,谢谢,很有帮助。
66
文章很好值得关注
56
#结直肠#
32
#重磅#
27
新治疗方法,
46
很不错,学习啦
0
谢谢分享,,,,,
47
很好,不错,以后会多学习
28