Blood:激酶抑制剂更佳序列治疗或为CLL患者带来持久的疗效
2016-10-21 MedSci MedSci原创
B细胞受体(BCR)激酶抑制剂(KI)代表了慢性淋巴细胞白血病(CLL)管理模式的转变,但是关于KI废止后的实践模式以及最佳的序列治疗的数据十分有限。在此多中心、回顾性研究中,研究人员纳入了178名CLL患者进行综合分析(ibrutinib = 143;idelalisib = 35),均停止了KI治疗治疗。研究人员探究了患者对KI治疗的反应,毒性,KI后的治疗,和总生存率(OS)。结果,患者治疗
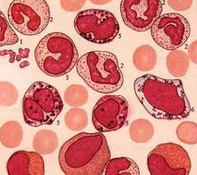
B细胞受体(BCR)激酶抑制剂(KI)代表了慢性淋巴细胞白血病(CLL)管理模式的转变,但是关于KI停药后的实践模式以及最佳的序列治疗的数据十分有限。
在此多中心、回顾性研究中,研究人员纳入了178名CLL患者进行综合分析(ibrutinib = 143;idelalisib = 35),均停止了KI治疗治疗。研究人员探究了患者对KI治疗的反应,毒性,KI后的治疗,和总生存率(OS)。
结果,患者治疗前的中位数为3(范围0-11);del17p(34%),p53基因突变(27%),del11q(33%),复杂核型(29%)。首次KI治疗后的总反应率(ORR)为62%(完全缓解(CR)14%)。KI停药的最常见的原因是治疗毒性(51%),CLL进展(29%),以及Richter转变(RT)(8%)。KI开始治疗后的中位无进展生存期(PFS)和OS分别为10.5个月和29个月。值得注意的是,最初KI的选择并不影响PFS或OS,但RT预示着显著低于OS(P = 0.0007)。114名患者停止KI治疗后接受了后续的抢救治疗,ORR至后续的KI为50%,中位PFS为11.9个月。KI不耐受而接受替代KI治疗的患者未达到中位PFS(范围为0.57-20个月)。然而,CLL进展首次接受KI治疗后来接受KI替代治疗的患者中位PFS为7个月(范围0.76-12月)。
总之,该研究表明,毒性是KI停药最常见的原因,那些因KI毒性而停药的患者对KI替代疗法反应较好,且这些反应较为持久。
原始出处:
Mato AR, et al. Outcomes of CLL patients treated with sequential kinase inhibitor therapy: a real world experience. Blood. 2016;doi:10.1182/blood-2016-05-716977.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








学习了谢谢作者分享!
57
#激酶抑制剂#
37
#抑制剂#
24
学习啦!分享一下!
50
可以借鉴一下!
51
专业性很强
49
#激酶#
20
慢性淋巴细胞白血病治疗
45
学习了啊
19
收藏
19