一例复发性胃出血的罕见原因
2018-06-23 江苏省人民医院消化科 消化客
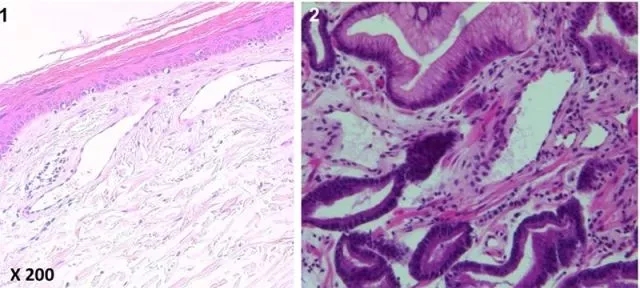
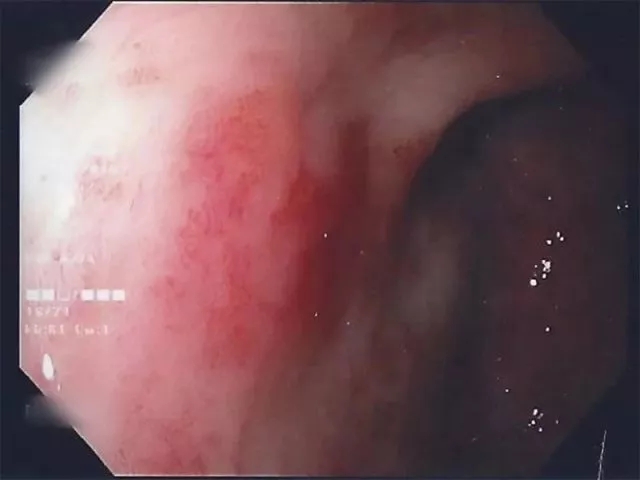
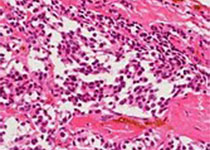
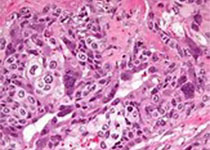
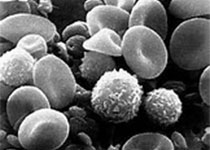
一名67岁女性因红血球容积达80 μg/l,气促,乏力,平均6 g/dl的低色素小细胞性贫血而入院。曾使用抗血小板药物治疗阵发性房颤(AF)。在过去的五年中,开始缓慢出现大量皮肤毛细血管扩张症状,从下肢延伸至大腿,臀大肌,躯干,背部,胸部和手臂(图A)。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#复发性#
39
#胃出血#
37
#罕见原因#
40
很好
52
#罕见#
31
阅
72