JAHA:外周动脉疾病患者感知与客观的步行能力变化
2021-06-03 MedSci原创 MedSci原创
运动显著改善了外周动脉疾病患者6分钟步行距离,但许多随机分配至运动组的参与者报告步行能力没有变化或下降。这些结果表明,相对于外周动脉疾病患者感知的步行改善,客观测量的步行改善水平与其存在显著差异。
在下肢外周动脉疾病患者中,运动对患者报告结局的影响尚未明确。

近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,来自于三项临床试验中的404 名外周动脉疾病患者被随机分为运动组(N=205)或对照组( N=199),并在基线和 6 个月的随访中完成了6分钟步行和步行障碍问卷距离评分(得分为0-100,100=最佳)。

与对照组相比,运动使患者6分钟步行距离提高了39.8 m(95%CI为26.8-52.8,P<0.001),步行障碍问卷距离评分提高了7.3分(95%CI为2.4-12.1,P=0.003)。在基线和随访中,总共有2828名受试者完成了步行障碍问卷距离评分。
两组6分钟步行距离比较
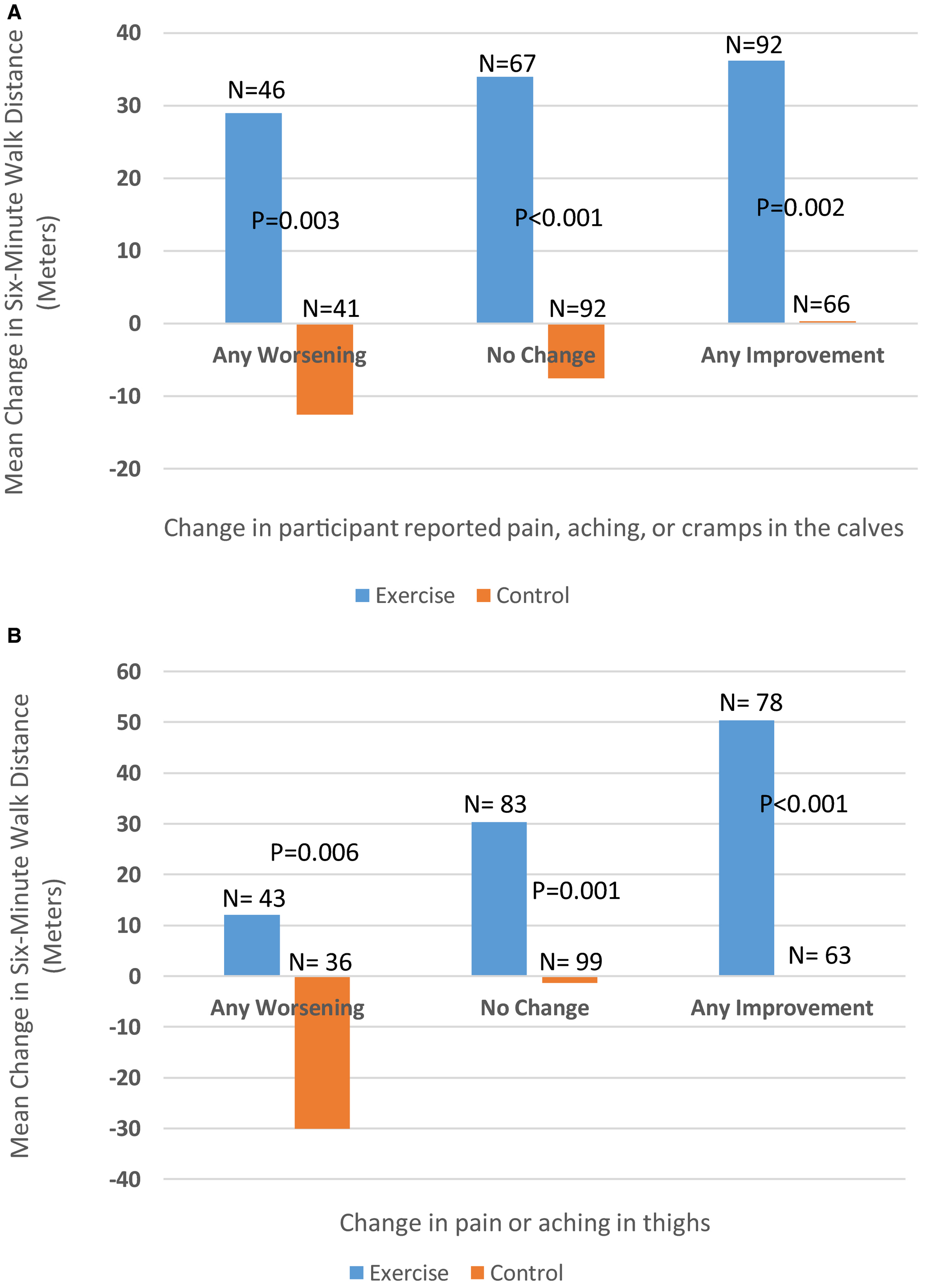
在基线和随访之间自我感知步行1m或更长距离的能力没有变化的参与者中,6 分钟步行在运动组中有所改善,而在对照组中有所下降(+26.8 vs. -6.5 m,P<0.001)。在基线和随访之间自我感知步行1m或更长距离的能力下降的参与者中,6 分钟步行在运动组中有所改善,而在对照组中有所下降(+18.4 vs. -27.3 m,P<0.001)。在随访时报告小腿症状恶化的参与者中,运动组有所改善,而对照组下降(+28.9 vs. -12.5 m,P<0.01)。
由此可见,运动显著改善了外周动脉疾病患者6分钟步行距离,但许多随机分配至运动组的参与者报告步行能力没有变化或下降。这些结果表明,相对于外周动脉疾病患者感知的步行改善,客观测量的步行改善水平与其存在显著差异。
原始出处:
Mary M. McDermott.et al.Perceived Versus Objective Change in Walking Ability in Peripheral Artery Disease: Results from 3 Randomized Clinical Trials of Exercise Therapy.J AM HEART ASSOC.2021.https://www.ahajournals.org/doi/full/10.1161/JAHA.120.017609
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#步行#
39
#疾病患者#
36
#AHA#
36
#外周动脉#
36