双C臂复合手术室在颅内外高流量搭桥术治疗颈内动脉海绵窦段巨大动脉瘤中的使用
2019-12-11 辛灿 章剑剑 李正伟 中国临床神经外科杂志
颈内动脉海绵窦段巨大动脉瘤采用单纯夹闭或者血管内治疗很难取得理想的疗效,应用颅内外高流量搭桥术治疗仍然是较好的选择。然而,无论是使用桡动脉还是大隐静脉作为桥血管,其通畅性在术中却很难得到直观的判断。复合手术室的投入使用能在术中实时观察血管通畅情况。
颈内动脉海绵窦段巨大动脉瘤采用单纯夹闭或者血管内治疗很难取得理想的疗效,应用颅内外高流量搭桥术治疗仍然是较好的选择。然而,无论是使用桡动脉还是大隐静脉作为桥血管,其通畅性在术中却很难得到直观的判断。复合手术室的投入使用能在术中实时观察血管通畅情况。
2017年8月至2017年12月在双C臂复合手术室内采用颅内外高流量搭桥术治疗5例颈内动脉海绵窦段巨大动脉瘤,现报道如下。
1. 临床资料
1.1 一般资料
5例均为女性;年龄29~77岁,平均54岁。头痛3 例,眼睑下垂1 例,眼周有麻木感1 例。病程10 d至20个月,平均7个月。
1.2 影像学资料
术前均行颅脑MRI平扫及增强扫描、CTA或DSA检查。DSA示5例均为颈内动脉海绵窦段巨大动脉瘤,右侧4例,左侧1例;动脉瘤大小(2.7 cm×2.3 cm)~(6.2 cm×4.1 cm)(图1A、1B)。
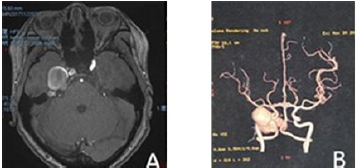
图1 A. 术前MRI;B. 术前CTA;
1.3 手术方法
全麻后,行DSA检查,后移开C臂常规取大隐静脉进行颅内外高流量搭桥术。在完成大隐静脉-颈外动脉、大隐静脉-大脑中动脉M2段端侧吻合后,再次行DSA检查。若桥血管狭窄或不显影,重新进行血管吻合,在DSA证实桥血管通畅后,结扎颈内动脉孤立动脉瘤,行最后一次血管造影(图1C、1D),确认桥血管通畅并且动脉瘤不显影。

图1 C.桥血管吻合后DSA;D.颈内动脉结扎后DSA;
2. 结果
术中DSA示有2例完成颅内外高流量搭桥术后桥血管显影欠佳,1例重新缝合颈外动脉-大隐静脉吻合口后通畅,另1例桥血管在拆开颈外动脉-大隐静脉和大隐静脉-大脑中动脉M2两处吻合口并再次吻合后显影。术后3例头痛较术前有明显缓解,另2例症状无明显变化;1例有轻度眼睑下垂,1例眼周麻木感仍然存在。5例术后头颅CTA示桥血管通畅。
3. 讨论
由于颈内动脉海绵窦段巨大动脉瘤位置深,周围结构复杂,颅内外高流量搭桥术能够在有效建立颅内外血供的同时孤立动脉瘤,达到良好的治疗效果。随着显微手术技术的提高以及各种手术设备的更新换代,颅内外高流量搭桥术得到了更加广泛的应用。采用颅内外高流量搭桥术治疗颈内动脉复杂动脉瘤的疗效是值得肯定的。然而,手术成功率主要取决于桥血管的通畅性,选择桥血管必须考虑到桥血管的长度、内径大小以及桥血管自身的病变和该血管取出后对其周围组织的影响。目前,常用的桥血管主要有大隐静脉和桡动脉。
Matsukawa等对使用桡动脉和大隐静脉行颅内外高流量搭桥术进行比较,认为桡动脉的通畅性要高于大隐静脉,对于Allen试验阳性的病人均应选择桡动脉行高流量搭桥术。国内也有学者采用桡动脉行高流量搭桥术,手术效果比较理想。而在选择大隐静脉进行颅内外高流量搭桥时,大隐静脉的主要来源是小腿。
Ramanathan等使用大隐静脉行高流量搭桥术并没有出现比使用桡动脉更高的桥血管闭塞率,原因可能是病例的大隐静脉来源于大腿,大腿的大隐静脉管壁更厚,管径更粗,同时将其吻合至M2最粗段,病人终身服用阿司匹林。此外,桡动脉比大隐静脉更容易发生血管痉挛,而且其取材长度也有限,同时远没有取大隐静脉方便。其实无论是选取大隐静脉或者是桡动脉行颅内外高流量搭桥术,治疗核心依然是保证桥血管的长期通畅。
目前,虽然术中荧光造影可以初步观察血管的吻合情况,但是利用显微镜的荧光技术仍然有较大的局限性,仅对术野表浅的血管显影良好,而且也不能观测到动脉瘤的变化情况。因而,术中脑血管造影技术的问世很好地解决了这一问题。现在配备有DSA机的神经外科复合手术室不仅可以进行介入诊断和治疗,还可以同时进行开颅显微手术,治疗复杂的脑血管病甚至脑肿瘤。
采用高流量搭桥术治疗颈内动脉海绵窦段巨大动脉瘤,复合手术室具有巨大优势。主要体现在术中造影可以即时观察血管通畅情况,在发现吻合口狭窄时能够及时地调整吻合口,同时减少了在多次转运病人时所带来的风险,缩短了手术时间,病人也更加安全。我们使用的是国际上先进的双C臂介入X线成像系统,比目前已有的单向复合手术室有更大的优势,不仅降低了造影剂用量和X线的剂量,介入操作更加方便快捷,而且给医护人员提供了更宽敞的操作空间。双向大面板能够提供更加高清的图像,还可以将3D血管影像和头颅Xper CT进行融合,更加准确地定位病变。
值得一提的是,复合手术室可以在术前对病人进行球囊栓塞试验后即刻决定手术方案,是单纯闭塞颈内动脉还是颅内外高流量搭桥治疗颈内动脉海绵窦段巨大动脉瘤作出选择。但是球囊闭塞试验的结果常常不可靠,假阴性结果的出现会给病人带来灾难性的后果。因此,无论试验结果阳性与否,都应进行血管重建术,建立新的颅内外循环,以确保病人的安全。
总之,应用双C臂复合手术室进行颅内外高流量搭桥术对确保术中桥血管的通畅是有效的,同时能够使病人更加安全。然而,在保证桥血管的长期通畅性上,我们仍要继续加强围手术期的治疗并且进行长期的随访,相信随着使用的熟练,复合手术室的应用会更加广泛。
原始出处:
辛灿,章剑剑,李正伟,熊忠伟,杨邦坤,吴小林,陈劲草.双C臂复合手术室在颅内外高流量搭桥术治疗颈内动脉海绵窦段巨大动脉瘤中的使用[J].中国临床神经外科杂志,2018(09):622-624.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#手术室#
39
#巨大动脉瘤#
26
#高流量搭桥术#
30
#颅内外#
37
#搭桥#
28
#搭桥术#
36
#颈内动脉#
42