JAMA Netw Open:基于网络的管理指南对2型糖尿病和糖尿病肾病患者危险因素的影响
2022-04-30 从医路漫漫 MedSci原创
在临床试验中,控制血压(BP)、血糖和血胆固醇水平以及使用肾素-血管紧张素-醛固酮系统(RAAS)抑制剂、钠-葡萄糖协同转运蛋白2抑制剂和finerenone已被证明可改善DKD患者的心血管和肾脏结果
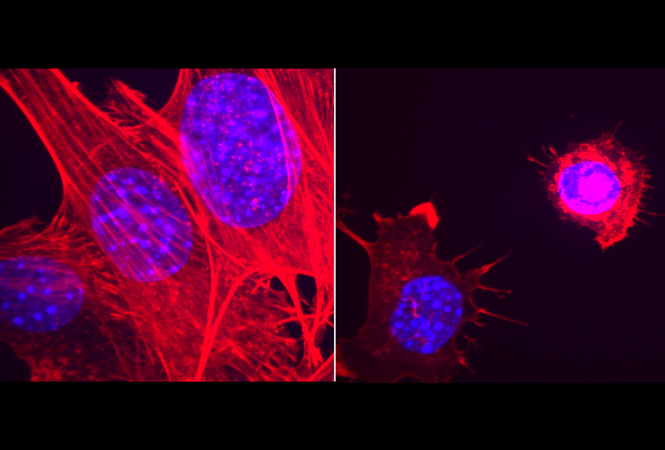
背景:糖尿病是全球慢性肾脏疾病和终末期肾脏疾病的主要原因。许多糖尿病性肾脏疾病(DKD)患者在肾脏替代治疗开始前死于心血管事件。在临床试验中,控制血压(BP)、血糖和血胆固醇水平以及使用肾素-血管紧张素-醛固酮系统(RAAS)抑制剂、钠-葡萄糖协同转运蛋白2抑制剂和finerenone已被证明可改善DKD患者的心血管和肾脏结果及存活率。例如,在亚洲,30%至40%的DKD患者达到了推荐的血糖和血压目标,50%的患者服用了RAAS抑制剂和他汀类药物。对181项涉及135 112名2型糖尿病患者的随机临床试验(RCT)的荟萃分析发现,团队护理、患者教育、自我管理支持和改善患者与临床医生的沟通在降低心脏代谢风险因素方面具有最大的效果,尤其是在亚洲等资源匮乏的地区,尽管缺乏DKD的证据。
DKD的早期发现、风险分层和及时管理的重要性需要更全面的实施战略。在亚洲进行的这项多中心随机对照研究中,我们旨在评估亚洲糖尿病联合评估(JADE)门户网站、护士提醒和团队护理对DKD患者多种危险因素的影响。我们假设JADE门户网站辅助的基于团队的护理以及定期反馈和患者赋权是改善这类患者群体的治疗目标实现和结果的可行策略。
目的:评价联合亚洲糖尿病评估(JADE)门户网站、护士提醒和团队护理对DKD患者多种危险因素的影响。
设计、设置和参与者:这项为期12个月的多国、开放标签随机临床试验于2014年6月27日至2019年2月19日在亚洲8个国家或地区的13个医院糖尿病中心进行。所有参与的患者都患有DKD。意向性治疗数据分析于2020年4月7日至6月30日进行。干预在每个研究点,患者以1:1:1的比例被随机分配到常规护理、授权护理或基于团队的授权护理。所有患者在基线和第12个月时都接受了JADE门户网站引导的结构化评估。常规护理组和授权护理组的患者接受了医学随访。授权护理组的患者也每3个月收到一份个性化的JADE报告和护士电话。以团队为基础的授权护理组的患者每3个月接受一次来自医护团队的面对面问诊。
主要结果和测量内容:主要结果是达到多重治疗目标的患者比例(定义为≥5个目标中的3个:HbA1c水平< 7.0% [53 mmol/mol],血压< 130/80 mm Hg,低密度脂蛋白胆固醇水平< 1.8 mmol/L,甘油三酯水平< 1.7 mmol/L,和/或持续使用肾素-血管紧张素-醛固酮系统抑制剂)。
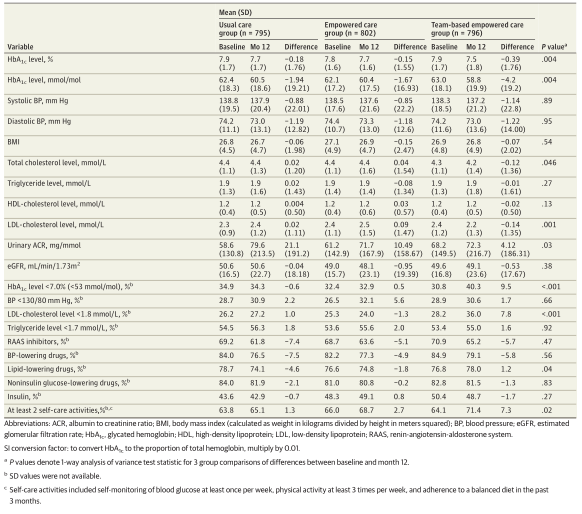
结果:共2393例患者(平均[SD]年龄,67.7 [9.8]岁;1267名男性[52.9%])被随机分配到常规护理组(n = 795)、授权护理组(n = 802)和团队授权护理组(n = 796)。在基线时,34.7%的患者(n = 830)接受3个治疗目标。在意向治疗分析中,以团队为基础的授权治疗组在实现多项治疗目标方面有进一步提高的患者比例最高(组内差异:常规治疗组,3.9% [95% CI,0.0%-7.8%];授权护理组,1.3% [95%可信区间为2.8%至5.4%];基于团队的授权护理组,9.1% [95%可信区间,4.7%-13.5%])。基于团队的授权治疗组比常规治疗组更有可能达到多重治疗目标(风险比[RR],1.17;95%可信区间,1.00-1.37)和授权护理组(RR,1.25;95%置信区间,1.06-1.48)。与未达到多重治疗目标的组相比,达到多重治疗目标的组报告了较低的心血管、肾脏和癌症事件发生率(8.4%[n = 51]vs 14.5%[n = 134];P = .004)。对符合方案人群的分析得出了类似的结果。
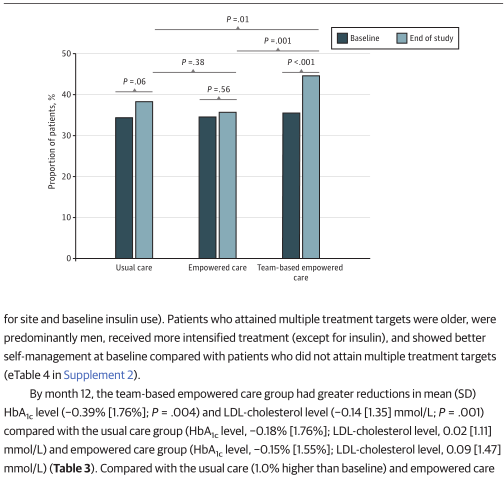
图1 意向治疗人群中在研究结束时达到至少3个治疗目标的患者比例的变化
表1 群体随机化效果对实现多重治疗目标的影响比较
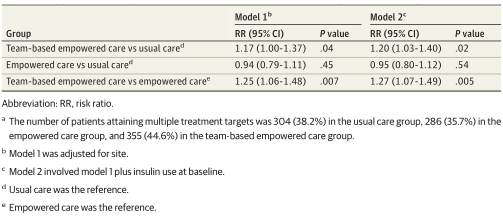
表2 .按治疗意向人群分组随机划分的基线至12个月期间心脏代谢危险因素和用药情况的变化
结论:该试验发现,为期12个月的技术辅助团队护理可以改善多种治疗目标。
原文出处: Chan JCN, Thewjitcharoen Y, Nguyen TK, Effect of a Web-Based Management Guide on Risk Factors in Patients With Type 2 Diabetes and Diabetic Kidney Disease: A JADE Randomized Clinical Trial.JAMA Netw Open 2022 Mar 01;5(3)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#PE#
31
#NET#
47
#管理指南#
47
#肾病患者#
42
这个研究不错,厉害了!!!谢谢分享
57
JAMA上文章都是顶级的,谢谢梅斯及时上新
29