斜坡骨巨细胞瘤1例
2018-12-20 李齐英 中国医学影像学杂志
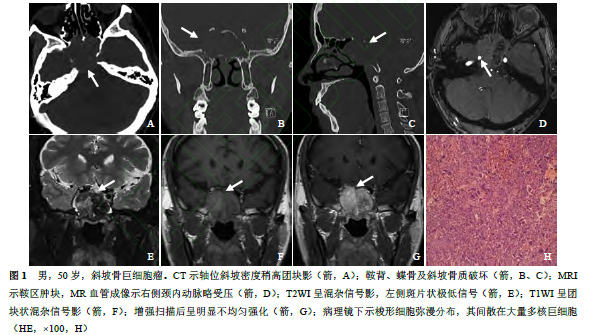
男,50岁,主诉:无明显诱因阵发性右侧头痛15d,加重伴右眼复视7d。影像学检查(图1A~G):CT见鞍区扩大,分叶状略高密度团块影突入蝶窦,鞍底下陷、鞍背变薄,蝶骨、枕骨斜坡骨质变薄,局部不连续;MRI提示斜坡、双侧蝶窦见团块状等、低混杂T1、T2信号影,边界不清,大小约3.6CM×3.6CM×4.7CM,左半病灶见斑片状稍长T1、短T2信号,增强扫描见明显不均匀强化,斜坡破坏,向后膨隆,右侧颈
病例简介
男,50岁,主诉:无明显诱因阵发性右侧头痛15d,加重伴右眼复视7d。影像学检查(图1A~G):CT见鞍区扩大,分叶状略高密度团块影突入蝶窦,鞍底下陷、鞍背变薄,蝶骨、枕骨斜坡骨质变薄,局部不连续;MRI提示斜坡、双侧蝶窦见团块状等、低混杂T1、T2信号影,边界不清,大小约3.6CM×3.6CM×4.7CM,左半病灶见斑片状稍长T1、短T2信号,增强扫描见明显不均匀强化,斜坡破坏,向后膨隆,右侧颈内动脉海绵窦段略受压。病理镜下图片见图1H。免疫组化:上皮膜抗原(-),波形蛋白(+),激素受体(-),胶质纤维酸性蛋白(-),S-100(-),P53(++),CD68(多核细胞+),P63(基质细胞+),Ki-67(局部15%+),CD34(血管+V0),平滑肌肌动蛋白(血管+)。诊断:(斜坡)巨细胞瘤,细胞增生活跃。
讨论
骨巨细胞瘤起源于中胚叶组织的成骨细胞,是一种局部侵袭性肿瘤,男女发病率相近,多发年龄为20~40岁。骨巨细胞瘤多发生于长骨的干骺端,发生于斜坡、肋骨等部位极少见。本例骨巨细胞瘤发生于斜坡。头痛是斜坡骨巨细胞瘤首先出现的临床症状,随后出现与肿瘤生长部位相关的颅神经受损表现,如肿瘤压迫两侧海绵窦内的II~VI颅神经,导致眼球活动和面部感觉障碍。当肿瘤累及垂体时可出现垂体功能异常;侵犯蝶窦甚至鼻腔时,引起嗅觉障碍和鼻塞。本例患者右眼复视,可能为右侧视神经受压迫所致。
斜坡骨巨细胞瘤呈浸润性缓慢生长,表现为骨源性软组织肿块,可见膨胀性、溶骨性骨质破坏,可侵蚀、破坏周围骨质。肿瘤内部较少发生钙化、出血和囊变,发生囊变时数量、大小不等,边界清晰。肿瘤典型的CT表现为广泛吸收性、膨胀性骨质破坏;增强扫描后肿块多数呈不同程度的不均匀强化。MRI无典型特征,T1WI上肿瘤可呈低信号、T2WI上呈低至中等信号,常表现为大小不等、边界清晰的混杂信号区。肿瘤血供丰富,增强扫描可见明显强化,如有散在分布的囊变、出血及钙化时,表现为斑片状、斑团状不均匀强化。
本例T1WI呈混杂稍低信号,右半部分T2WI呈混杂信号,与既往报道的MRI表现相似,病变左半部分T2WI呈低信号,不均匀强化的程度小于右半病变,考虑为肿瘤内部亚急性出血所致。斜坡骨巨细胞瘤一般不出现“皂泡样”改变,影像学诊断相对困难,需与脊索瘤、软骨肉瘤相鉴别。三者均以溶骨性、膨胀性骨破坏及侵蚀邻近骨质为特点,区别在于脊索瘤内有大量黏液成分,可有点片状钙化,因此MRI上T1WI呈不均匀混杂信号,T2WI呈不均匀高信号,不均匀蜂房样、颗粒样强化;斜坡软骨肉瘤呈偏心性生长,MRI表现为低或稍低T1信号,T2高信号,病灶内可出现钙化低信号,轻中度强化,压脂和梯度回波序列可见高信号的软骨成分。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#细胞瘤#
25
#骨巨细胞瘤#
52
#巨细胞#
45