南京医院学者Meta分析研究显示:一成TAVR术后患者将新发房颤
2016-12-02 朱灏, 任晓敏, 蔡金赞, 等. 中国循环杂志, 2016, 31: 11
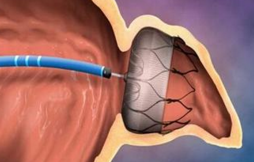
经导管主动脉瓣置换术(TAVR)后新发房颤逐渐引起关注。南京医科大学附属南京医院张瑶俊、朱灏等进行的Meta分析研究发现,TAVR术后新发房颤并不少见,发生率为11.1%。 此外,经心尖途、手术相关心脏事件、手术相关出血事件、心房过大(每增加1 mm/m2),均是TAVR术后新发房颤的独立预测因素。 而且,这些因素均有相应引起房颤的机制。比如经心尖途径容易引起新发房颤可能与胸廓
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Meta#
28
跟技术有没有关系
55
#AVR#
33
#MET#
35
#新发房颤#
27
经导管主动脉瓣置换术(TAVR)后新发房颤逐渐引起关注,TAVR术后新发房颤并不少见,发生率为11.1%。
61
值得关注
56