Lancet Respirat Med:长期应用ASK1抑制剂Selonsertib是否可降低PAH患者的肺血管阻力?
2021-08-21 Nebula MedSci原创
预临床实验表明,氧化应激和ASK1活性增强可能在肺动脉高压 (PAH) 的病理过程中起重要作用,那长期应用ASK1抑制剂Selonsertib是否可降低PAH患者的肺血管阻力?
从人肺组织和临床前模型中获得的数据表明,氧化应激和细胞凋亡信号调节激酶 1 (ASK1) 活性增强可能在肺动脉高压 (PAH) 的病理过程中起重要作用。本研究的目的是确定 ASK1 抑制剂 Selonsertib 与安慰剂相比在 PAH 患者中的疗效、安全性和耐受性。
这是一项在多个国家的46个中心开展随机、双盲、安慰剂为对照的2期试验,招募了18-75岁的确诊的特发性或遗传性PAH,或与结缔组织病、药物或毒素、人类免疫缺陷病毒或修复的先天性心脏缺陷相关的 PAH患者。受试患者被1:1:1:1随机分至4组,接受安慰剂或2 mg、6 mg 或 18 mg的Selonsertib(每日口服)。主要终点是24周时肺血管阻力的变化。
2014年12月3日-2015年11月13日,共招募了151位患者,其中150位接受了Selonsertib或安慰剂,134位(89%)完成了24周的研究治疗;所有人都在接受背景 PAH 治疗(138位[92%]在接受联合治疗)。90位(60%)患者肺功能II级,60位(40%)肺功能III级。基线平均肺血管阻力为772 (SD 334) dyn·s/cm5。
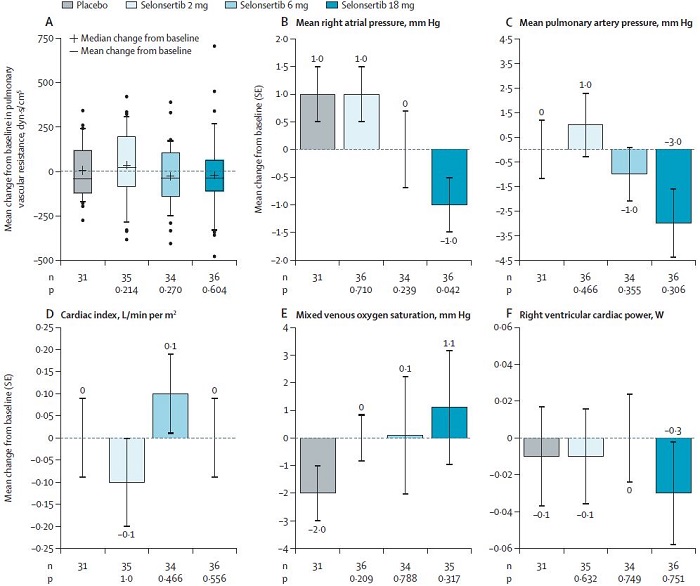
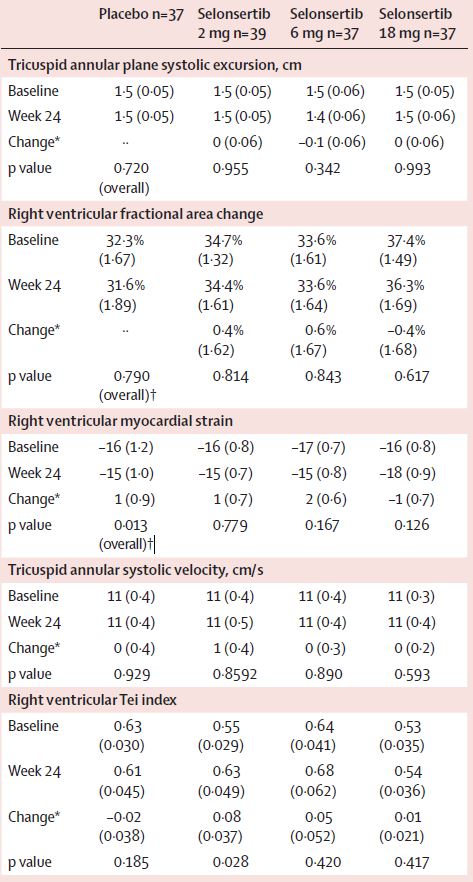
24周时各组肺血管动力的各参数的变化
24周时,安慰剂组、2 mg Selonsertib组、6 mg Selonsertib组和18 mg Selonsertib组的平均肺血管阻力变化分别是6.0 dyn·s/cm5 (SD 28.0; n=31)、35.0 (35.4) dyn·s/cm5 (n=35; 与安慰剂相比 p=0.21)、-28.0 (30.2) dyn·s/cm5 (n=34; 与安慰剂相比 p=0·27)和-21.0 (37.9) dyn·s/cm5 (n=36; 与安慰剂相比 p=0.60)。
不良反应事件
Selonsertib组最常见的不良反应事件有头疼(17例[15%])、怪梦(8[7%])、恶心(7[6%])和腹泻(7[6%]);安慰剂最常见的不良反应事件有头疼(6[16%])、恶心(5[14%])和腹泻(2[5%])。113位采用Selonsertib治疗的患者中有23位(20%)报告了严重不良反应事件,接受安慰剂的37位患者中有7位(19%)。
总之,连续24周应用Selonsertib(1/日)并不能显著显著降低PAH患者的肺血管阻力或改善临床情况,但安全性和耐受性良好。
原始出处:
Stephan Rosenkranz, et al. Selonsertib in adults with pulmonary arterial hypertension (ARROW): a randomised, double-blind, placebo-controlled, phase 2 trial. The Lancet Respiratory Medicine. August 21, 2021. https://doi.org/10.1016/S2213-2600(21)00032-1
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#抑制剂#
29
#Selonsertib#
36
#ASK1#
45
#Lancet#
43
#肺血管阻力#
56
#PAH#
48
#Med#
29
学习
38
顶刊就是不一样,质量很高,内容精彩!学到很多
46