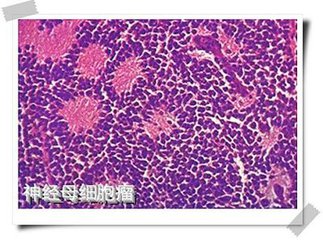
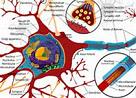
Nat Commun:中山大学朱孝峰教授团队发现调控神经母细胞瘤分化的重要机制和新靶标
2017-11-03 佚名 细胞
2017年10月27日,国际学术权威刊物自然出版集团旗下子刊《Nature Communication》杂志在线发表了中山大学华南肿瘤学国家重点实验室朱孝峰教授团队题为“CaMKII-mediated Beclin 1 phosphorylation regulates autophagy that promotes degradation of Id and neuroblastoma cell
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#母细胞瘤#
25
#Nat#
0
#COMMUN#
42
#靶标#
30
#细胞瘤#
31
#中山大学#
27