JACC:预测急性心衰患者的肾功能恶化——NGAL效果较差
2016-09-25 MedSci MedSci原创
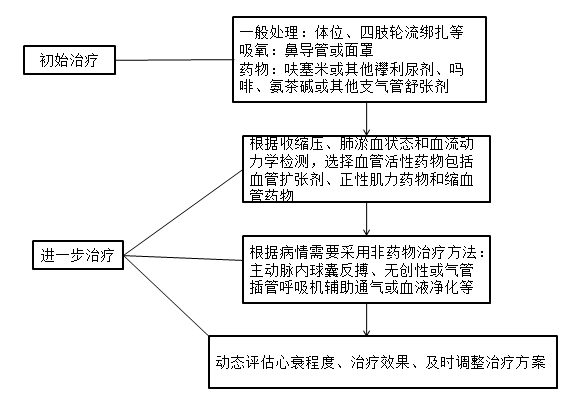
急性心衰(AHF)期间经常出现肾功能恶化(WRF),这预示着不良结局;因此,及早识别可能有助于降低风险。嗜中性粒细胞明胶酶相关脂质运载蛋白(NGAL)是一种新型的肾生物标志物,在某些疾病中可以预测WRF,但其在AHF中的价值还是未知的。这项研究旨在确定,在静脉注射利尿剂治疗的AHF患者中,对于预测WRF和或其进展,NGAL是否优于肌酐。来自美国的研究人员开展了一项多中心,前瞻性队列研究,该研究招募
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#肾功能#
24
急性肾衰竭!学习!
73
了解一下!分享一下!
67
#JACC#
34
总结的很好!
79
分享一下!
64
谢谢分享,学习了。
78
谢谢分享,学习了。
22
谢谢分享,学习了。
28
谢谢分享,学习了。
26