Stroke:他汀类药物的依从性与有或无房颤患者复发卒中风险降低有关!
2017-06-09 xing.T MedSci原创
由此可见,服用他汀类药物的依从性与降低卒中复发风险之间的相关性在房颤患者和非房颤患者中一样强烈,提示房颤状态不应该是一个排除他汀类药物用于患者脑卒中的二级预防的原因。
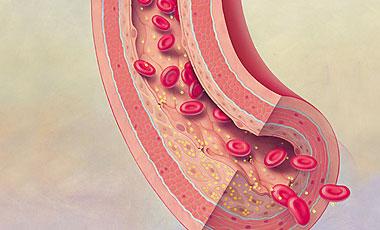
门诊使用他汀类药物可以降低血栓引起的脑卒中患者缺血性卒中复发风险。但他汀类药物对心房颤动所致的缺血性脑卒中患者是否具有相似的作用尚不清楚。
近日,卒中领域权威杂志Stroke上发表了一篇研究文章,研究人员旨在对门诊患者服用他汀类药物的依从性,通过覆盖天数的比率来衡量,与患有或不患有房颤的患者发生复发性缺血性卒中风险之间的相关性进行评估。
在6116例缺血性脑卒中出院后服用他汀类药物5年的患者中,1446例(23.6%)患者在出院时被诊断为房颤。他汀类药物的平均依从率(覆盖天数比率)为85,研究人员发现高水平的覆盖天数比率与较大的低密度脂蛋白抑制程度相关。在超过3年的复发性缺血性脑卒中多变量生存模型中,在控制了年龄、性别、种族/民族、并发症和中心医院后,他汀类药物依从性较高可以预测不患有(风险比为0.78;95%可信区间为0.63-0.97)或患有(风险比为0.59;95%可信区间为0.43-0.81)房颤患者降低的卒中风险。在服用华法林的房颤患者中调整国际标准化比值时间到治疗范围后,这种相关性仍然明显(风险比为0.61;95%可信区间为0.41-0.89)。
由此可见,服用他汀类药物的依从性与降低卒中复发风险之间的相关性在房颤患者和非房颤患者中一样强烈,提示房颤状态不应该是一个排除他汀类药物用于患者脑卒中的二级预防的原因。
原始出处:
Alexander C. Flint, et al. Statin Adherence Is Associated With Reduced Recurrent Stroke Risk in Patients With or Without Atrial Fibrillation.Stroke. 2017. https://doi.org/10.1161/STROKEAHA.117.017343
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#他汀类药#
0
#风险降低#
48
#卒中风险#
45
#依从性#
35
#房颤患者#
39
值得关注,感兴趣
53