EBioMedicine:孕期酒精暴露和青春期应激对成年雌性大鼠关节炎反应的调节作用
2022-03-06 医路坦克 MedSci原创
基于初步临床数据显示胎儿酒精谱系障碍(FASD)的个体患自身免疫性疾病的风险较高,本研究在佐剂性关节炎大鼠模型中研究了产前酒精暴露(PAE)对炎症性疾病分布的调节影响。
类风湿性关节炎是关节炎的慢性炎症性疾病,全球患病率约为0.24%.然而,某些亚组的类风湿性关节炎患病率要高达4%。此外,虽然已经确定了类风湿性关节炎的遗传脆弱性,并且越来越多的已知环境风险因素和类风湿性关节炎的触发因素,如吸烟,肥胖和近期感染,尚不清楚产前环境是否会影响类风湿性关节炎等自身免疫性疾病的晚年风险。
本研究利用我们完善的产前酒精暴露(PAE)动物模型,使用远交大鼠品系(Sprague-Dawley)研究这种产前环境损害对佐剂诱导的关节炎的发病率,严重程度和病程的影响。该PAE动物模型用于研究胎儿酒精谱系障碍(FASD),其是指与人类怀孕期间酒精暴露相关的广泛缺陷。作为人类类风湿性关节炎的模型,我们在这里使用啮齿动物佐剂诱导的关节炎模型,这是一种快速发作的T细胞依赖性炎症模型,导致关节炎症(约40-60%的动物),特别是后爪关节,注射后约10天开始,注射后约16天达到峰值(根据大鼠的应变,剂量和注射方式而变化).10-13天后爪关节的组织病理学和放射学检查通常在第15天确定关节损伤和畸形,注射后活动性慢性炎症阶段通常持续约35天。
已经确定的是,对于类风湿性关节炎等自身免疫性疾病,下丘脑-垂体-肾上腺(HPA)轴与免疫系统之间的通信发生改变,并且这可能导致疾病发作和发展轨迹。因此,对改变的HPA免疫相互作用的研究与阐明PAE后自身免疫性疾病增加的潜在机制特别相关。
在这里,我们使用“多次打击”或累积应激的概念来评估PAE和青少年应激对关节炎结局可能的独立和交互影响。这一概念表明,早年的不良经历,在这种情况下,酒精暴露(第一次),程序生理系统,导致改变HPA/免疫敏感性和增加对晚年生活挑战的反应性(第二次和第三次)。因此,在PAE后,一半的大鼠暴露在慢性温和应激(CMS)下,另一半的大鼠在青春期保持不受干扰。基于我们之前的发现,PAE会导致更严重和更长的关节炎病程,我们在炎症高峰期和康复后终止了动物。我们假设PAE会导致更严重的关节炎和关节炎的恢复受阻,这会因青少年压力而进一步恶化。此外,我们预计PAE大鼠的关节炎严重程度、HPA活性、关节完整性和炎症之间存在不匹配。临床相关指标(激素和免疫标记物以及胫跖关节的组织病理学)的使用使我们能够洞察预测PAE大鼠对炎症的高度敏感性的因素。重要的是,在PAE模型中洞察关节炎的生理基础不仅可以改善FASD患者的治疗,还可以更广泛地理解类风湿性关节炎的环境风险因素。
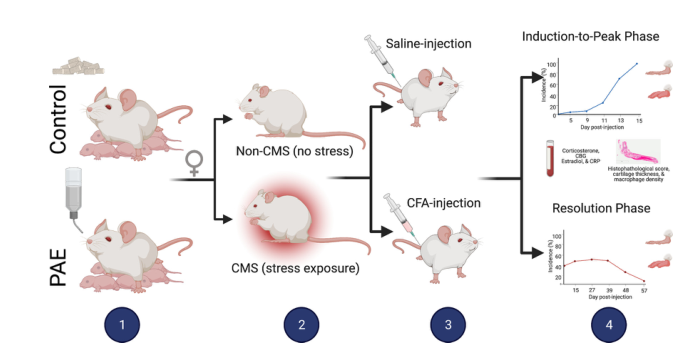
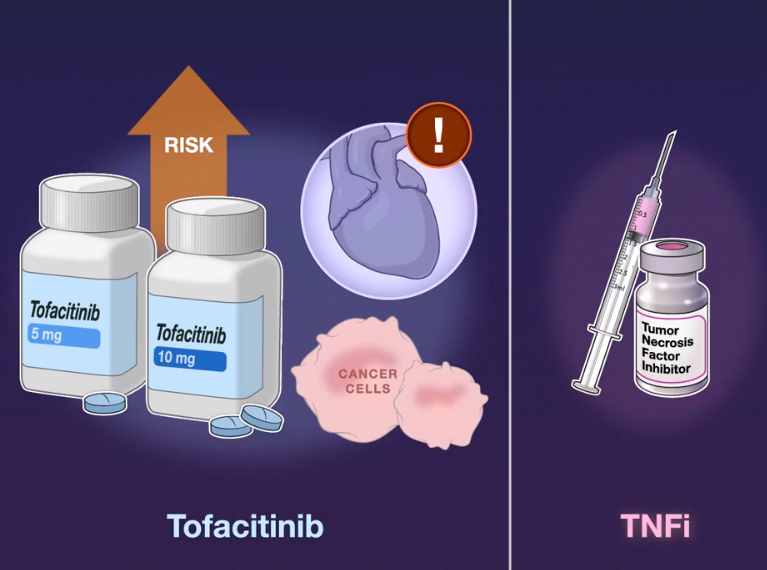
图1.研究概述1:在怀孕期间(GD1-21)给怀孕母鼠喂食(液体乙醇或颗粒状对照);2:青春期女性从p31?41开始暴露于慢性温和应激(CMS)或不受干扰(Non-CMS);3:成年大鼠(p55-60)在尾部皮内注射完全弗氏佐剂(CFA)或生理盐水;4:在第5、9、11、13、15天评估关节炎的严重程度。大鼠要么在关节炎高峰期(注射后第16天)被终止,要么随后被终止(在关节炎恢复后终止)。测定血浆皮质酮、CBG、雌二醇和CRP水平,评估所有动物后爪的关节炎严重程度(组织病理学评分)、软骨厚度和巨噬细胞密度。PAE:产前酒精暴露;CMS:慢性轻度应激;CRP:C反应蛋白。
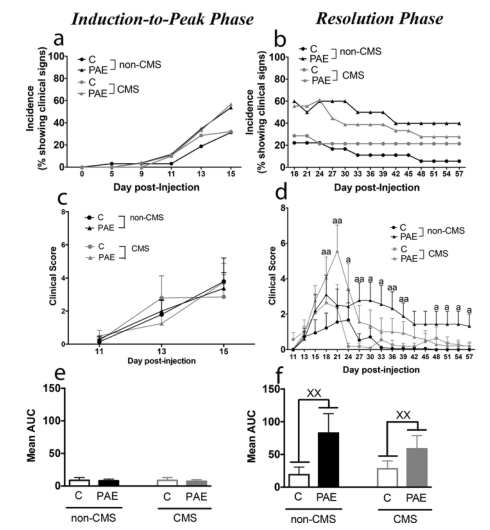
图2 关节炎的临床过程a,b:在诱导-高峰阶段(a)和分辨阶段(b)期间显示关节炎临床症状的佐剂注射大鼠的关节炎发生率。c、 d:在诱导至峰值阶段(c)和分辨阶段(d)期间发生关节炎的大鼠的平均临床评分(§SEM)。e、 f:诱导至峰值阶段(e)和分辨阶段(f)期间平均临床评分的曲线下面积(AUC;平均值§SEM)。在分辨阶段,与应激条件下的C大鼠相比,PAE中的AUC更高。“a”:产前治疗-日间互动;“£”:产前治疗的主要效果。统计检验(a?d):方差分析;e、 f:曲线下面积(AUC)。显着的事后比较:一个符号:p<0.05;两个符号:p<0.01;盐水:n=6/产前治疗/压力状况/时间点;注射佐剂:n=14/产前治疗/压力状况/时间点。C: 控制;PAE:产前酒精暴露;非CMS:无压力条件;CMS:压力条件。
已知的环境风险因素与类风湿性关节炎相关;然而,关于产前环境如何影响类风湿性关节炎的后世风险,我们知之甚少。基于初步临床数据显示胎儿酒精谱系障碍(FASD)的个体患自身免疫性疾病的风险较高,本研究在佐剂性关节炎大鼠模型中研究了产前酒精暴露(PAE)对炎症性疾病分布的调制影响。
怀孕大鼠在整个妊娠期间接受液体乙醇或对照饮食。为了模拟FASD患者经常经历的压力源暴露增加,青春期后代暴露于慢性轻度压力(CMS)或保持不受干扰。在成年期,开始实验性关节炎并且大鼠在炎症的峰值或消退后终止以评估内分泌,免疫和组织病理学结果。
PAE大鼠的关节炎发病率和严重程度增加,恢复受损。即使面对关节炎临床症状的明显恢复,在PAE动物中也观察到关节损伤增加,而似乎雌二醇可能具有保护作用。此外,随着PAE和青少年压力的组合,在PAE的滑膜中检测到增加的巨噬细胞密度,但在对照大鼠中未检测到。
这些发现表明,PAE改变了关节炎的严重程度和病程,突出了不良产前暴露对免疫调节的潜在影响。特别是,这些数据对理解初步数据有一定的意义,这些数据表明FASD患者自身免疫性疾病的倾向增加。
文献来源:Bodnar TS, Mak DY, Hill LA, Modulatory role of prenatal alcohol exposure and adolescent stress on the response to arthritis challenge in adult female rats.EBioMedicine 2022 Feb 17;77
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#DIC#
42
#Bio#
36
#CIN#
29
#EBI#
61
#关节炎#
24
#青春期#
40
#应激#
51
#Medicine#
28
#Med#
35
学习
55