重磅!科学家质疑巨病毒存在类似CRISPR/Cas的系统
2016-07-08 佚名 生物谷
在很多细菌中发现的CRISPR/Cas免疫防御系统,因其能够简单地而又优雅地编辑宿主基因组,而成为时下最火热的生物技术,在近期产生一大批发现。在今年3月,来自法国艾克斯-马赛大学的Didier Raoult和同事们发表一篇论文,指出一种被称作mimivirus的巨病毒(giant virus)拥有一种类似于CRISPR系统的被称作mimivirus噬病毒体抵抗元件(mimivirus vir
在很多细菌中发现的CRISPR/Cas免疫防御系统,因其能够简单地而又优雅地编辑宿主基因组,而成为时下最火热的生物技术,在近期产生一大批发现。在今年3月,来自法国艾克斯-马赛大学的Didier Raoult和同事们发表一篇论文,指出一种被称作mimivirus的巨病毒(giant virus)拥有一种类似于CRISPR系统的被称作mimivirus噬病毒体抵抗元件(mimivirus virophage resistance element, MIMIVIRE)的噬病毒体抵抗机制(Nature, 10 March 2016, doi:10.1038/nature17146)。而在上个月发表在Virologica Sinica期刊上的一篇论文中,来自法国国家科学研究院(CNRS)的Jean-Michel Claverie和Chantal Abergel对这种观点提出挑战。
Claverie和Abergel在他们的论文中写道,“MIMIVIRE并不类似于CRISPR-Cas系统,并不能够作为一种核酸识别系统发挥作用,也不可能拥有一种真正的适应性免疫系统所拥有的所有性质。”
Claverie和Abergel继续质疑这种噬病毒体抵抗机制到底是不是基于核酸的。他们提出蛋白可能干扰这种抵抗噬病毒体的mimivirus中的噬病毒体复制。
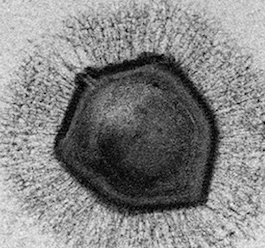
巨病毒因大的尺寸和巨大的基因组而得名。它们栖息在阿米巴变形虫中,而且能够被噬病毒体感染。Raoult和同事们在1992年在研究一座水冷却塔中的肺炎暴发时发现了mimivirus的病毒科Mimiviridae。他们起初把它们错认为是细菌,但是实际上是病毒。
为了验证提出的一个假设:mimivirus拥有一种类似于在细胞中发现的CRISPR/Cas系统的防御机制,Raoult和同事们对45种新的mimivirus毒株的DNA进行测序。他们在60种mimivirus的基因组中寻找能够与在Zamilon---一种感染一些mimivirus毒株(谱系B和C)的噬病毒体---基因组中发现的序列相匹配的序列。他们发现属于谱系A的mimivirus毒株抵抗Zamilon感染,含有Zamilon基因组中的一个重复序列,他们将它称作为MIMIVIRE。当让这个重复序列沉默时,他们发现这能够让这种病毒容易遭受噬病毒体感染。
但是,Claverie和Abergel声称这种mimivirus防御机制一点都不像CRISPR系统。首先,mimivirus基因组和噬病毒体复制发生在相同的地方,“这就不可能获得基于核酸的免疫系统”。再者,CRISPR代表着规律间隔性成簇短回文重复序列,而MIMIVIRE序列“并不是规律间隔性的,而且在两侧也不存在可识别的重复序列”。最后,与MIMIVIRE序列相对应的Zamilon序列缺乏被称作前间隔序列邻近基序(protospacer adjacent motif, PAM)的序列,其中细菌宿主通常利用这一序列区分病原体DNA和它们自己的DNA。
Raoult告诉《科学家》杂志,“它当然不是CRISPR。这是一种类比,而不存在同源性。”
其他没有参与这项研究的病毒学家也赞同Claverie和Abergel提出的批评意见。
来自美国洛克菲勒大学的Luciano Marraffini在发给《科学家》杂志的电子邮件中写道,“尽管MIMIVIRE明显作为一种抗噬病毒体系统发挥作用,但是它似乎缺乏CRISPR-Cas系统的一些典型特征,如存在被短病毒序列间隔开的重复序列阵列,使用短片段RNA作为向导RNA。”
来自美国北卡罗莱纳州立大学的Rodolphe Barrangou对此表示赞同。他在发给《科学家》杂志的电子邮件中写道,认为MIMIVIRE系统类似于CRISPR“走得太远了”。
另一种批评意见最初是由研究论坛PubPeer上的一名匿名的评论员提出的。它指出Raoult和同事们的研究缺乏RNA沉默对照实验,因而不能排除观察不到噬病毒体感染可能是由于mimivirus只是未发生复制。
Barrangou说,“并不存在CRISPR,也不存在Cas。对MIMIVIRE而言,这种类似性存在着偶然因素。我殷切希望科学家们保持开放心态,但是他们未免想象得有点儿太丰富了。”
原始出处
Jean-Michel Claverie, Chantal Abergel.CRISPR-Cas-like system in giant viruses: why MIMIVIRE is not likely to be an adaptive immune system.Virol Sin. 2016 Jun
Anthony Levasseur, Meriem Bekliz, Eric Chabrière, Pierre Pontarotti, Bernard La Scola & Didier Raoult.MIMIVIRE is a defence system in mimivirus that confers resistance to virophage.Nature. 2016 Mar 10;
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#质疑#
38
学习了,很深入
129
#CRISPR#
30
#重磅#
31
#Cas#
38