ANN ONCOL:循环肿瘤DNA追踪转移性乳腺癌芳香酶抑制剂耐药演变
2018-01-23 MedSci MedSci原创
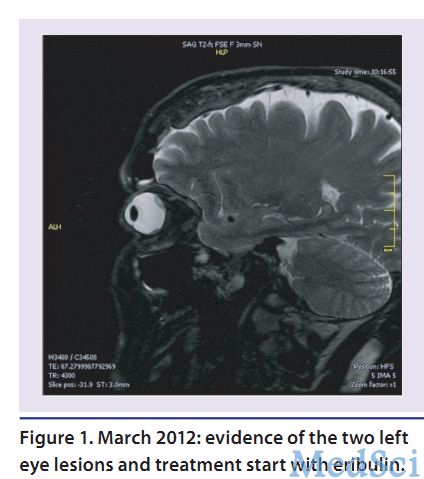
耐药突变在内分泌治疗耐药发展过程中扮演了重要的角色。ESR1突变在原发乳腺癌中很少见,但是在接受芳香酶抑制剂(AI)治疗的晚期乳腺癌患者中常见。ANN ONCOL近期发表了一篇文章,通过对晚期乳腺癌患者进行ctDNA连续性检测研究一线AI治疗耐药的演变过程。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#芳香酶抑制剂#
29
#抑制剂#
27
#Oncol#
30
#演变#
31
#转移性#
36
#循环肿瘤DNA#
38
henhao
0
不错的文章值得推荐
62
henhao
65
henhao
63