携带EGFR突变的非小细胞肺癌软脑膜转移(LM)更常见,且对TKI治疗反应好
2016-08-18 MedSci MedSci原创
广东省肺癌研究所、广东省人民医院吴一龙教授团队近日在《胸部肿瘤学杂志》(J Thor Oncol,JTO)发表研究论文,研究发现,在表皮生长因子受体(EGFR)基因突变非小细胞肺癌(NSCLC)患者中,柔脑膜转移(LM)更为常见。与未接受酪氨酸激酶抑制剂(TKI)治疗的患者相比,接受TKI治疗者的总生存(OS)期更长,提示TKI治疗LM的有效性。吴一龙教授柔脑膜是覆盖大脑的薄膜,包括蛛网膜和软脑膜
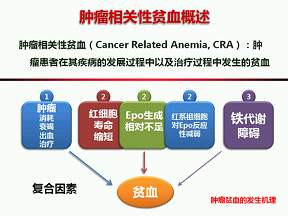
广东省肺癌研究所、广东省人民医院吴一龙教授团队近日在《胸部肿瘤学杂志》(J Thor Oncol,JTO)发表研究论文,研究发现,在表皮生长因子受体(EGFR)基因突变非小细胞肺癌(NSCLC)患者中,柔脑膜转移(LM)更为常见。与未接受酪氨酸激酶抑制剂(TKI)治疗的患者相比,接受TKI治疗者的总生存(OS)期更长,提示TKI治疗LM的有效性。

吴一龙教授在采访中谈到:
作者认为:
“尽管仍有局限,此项研究显示的LM后OS期比既往报道更长,且携带EGFR突变基因的NSCLC患者LM更为常见。EGFR TKI是EGFR突变LM患者的最佳治疗策略,尤其是针对TIK初治患者。然而,无论是否联合EGFR TKI,此项研究并不支持积极的全脑放疗。
另外,我们启动的比较EGFR TKI埃可替尼和全脑放疗的头对头前瞻性随机对照研究BRAIN,也将在12月份的世界肺癌大会(WCLC)上公布结果。”
本文参考:Leptomeningeal Metastases Are More Common inNSCLC Patients Harboring EGFR Mutationsand Respond Positively to TKI Therapy. Written by: Jacinta Wiens, PhD
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#软脑膜#
49
#非小细胞#
32
不错,
65
这篇资讯写的真好,带给我们新知识,启发新思维,不论是科研还是临床工作都有很大的帮助。。。
77
这篇资讯写的真好,带给我们新知识,启发新思维,不论是科研还是临床工作都有很大的帮助。。。
65
学习了!!?
67
#TKI#
42
#GFR#
30
值得学习
67
值得学习
27